MedFriendly®


Interstitial Pneumonia
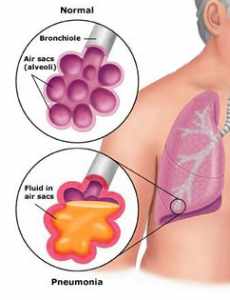
To begin with, pneumonia is inflammation of the lungs due to
infection. The lungs are two organs in the body that help people
breathe. Interstitial pneumonia is a long-term inflammatory lung
disease that affects the interstitial (connective) tissue of the
lungs. The inflammation is due to the build up of white blood cells
and protein-rich plasma (the watery part of blood) throughout the
alveoli. White blood cells help protect the body against diseases
and fight infections. Alveoli are tiny sacs where gases are
exchanged in the lungs so that breathing can take place. The
inflammation in interstitial pneumonia extends beyond the end of
the bronchioles. Bronchioles are small airways that branch off
the other small airways connected to the lungs. These other
small airways are known as bronchi.
FEATURED BOOK: Pneumonia in Children: Prevention & Treatment
The inflammation in interstitial pneumonia extends beyond the end of the bronchioles.
Bronchioles are small airways that branch off the other small airways connected to the
lungs. These other small airways are known as bronchi.
If the inflammation lasts long enough it can cause fluid in the lungs to harden, resulting in
the production of firm connective tissue (scar tissue). The production of this firm tissue is
known as fibrosis. There is also collagen formation in the walls of the alveoli. Collagen is
a fiber-like protein found in the skin.
"Where Medical Information is Easy to Understand"™
If the scar tissue formation is extensive enough, the alveoli may be
destroyed over time and the resulting space can be taken over by
cysts. A cyst is an abnormal lump, swelling, or sac that contains
fluid, a part solid material, or a gas, and is covered with a
membrane. A membrane is a thin layer of flexible tissue that covers
something. As the disease progresses, the bronchi and the walls of
the bronchi eventually become widened, the walls of the bronchi are
destroyed, and the lungs shrink. When patients with interstitial
pneumonia die and the lungs are examined, there are characteristic
large cells found lining the alveoli. The giant cells that line the alveoli
have multiple nuclei. A nucleus is the structure at the center of a
cell.
More than one nucleus is known as nuclei. The presence of these large cells in the alveoli is why
interstitial pneumonia is also known as giant cell pneumonia. Interstitial pneumonia is most common
between the ages of 40 and 70.
ARE THERE DIFFERENT TYPES OF INTERSTITIAL PNEUMONIA?
Yes. There are different types of interstitial pneumonia which are each sufficiently different enough from
each other to be considered distinct diagnoses. The different types of interstitial pneumonia are described
below:
USUAL INTERSITIAL PNEUMONIA (UIP): This is the most common type of interstitial pneumonia. UIP is
a deadly disease that commonly occurs in people 60 years or older that were otherwise in good health. It
is not uncommon in the 5th decade of life. Males and females are affected in equal numbers.
UIP begins slowly, with inflammation of the alveoli and increased numbers of cells in the walls of the
alveoli. Alveoli are tiny sacs where gases are exchanged in the lungs so that breathing can take place. As
the disease progresses, it becomes more difficult to breath. By the time the diagnosis is made, breathing
ability has significantly decreased.
The lung tissue will have an abnormal, honeycombed appearance, much like a bee hive. This is due to the
disease causing patchy distortion and destruction of the lung tissue structure. The honeycombs are
actually holes in the lung that are about one centimeter wide. The presence of honeycombs usually
represents the end stage of many forms of lung disease. In about half of UIP patients, x-rays of the lungs,
show hazy appearance of ground glass in the lungs. The ground glass appearance is known as ground
glass opacities and is usually due to inflammation of the alveoli, thickening of the alveoli walls, or early
fibrosis (an overgrowth of connective tissue).
The ends of the fingers are enlarged in about 83% of patients with UIP. Small amounts of old fibrosis (see
above) are also present. There is also recent granulation tissue present. Granulation tissue is new
connective tissue and tiny blood vessels that is commonly seen on the surfaces of wounds during the
healing process. About 7% of patients with late-stage UIP have a pneumothorax noticeable on x-ray. A
pneumothorax is the presence of air or gas in the pleural space, causing a lung to collapse. Part of the
lung tissue will also look normal in UIP. In about 6% patients with UIP, the pleura often appears thickened
on X-ray. The pleura is the smooth, moist double layer of flexible tissue that lines the lungs and the chest
wall.
In about 4% of UIP cases, X-rays show pleural effusions, which is the buildup of fluid in the pleural spaces
of the lungs. The pleural space is a thin, fluid-filled opening between the pleura of the lungs and the pleura
of the chest wall. Over time, lung size decreases in UIP, which can also be seen on x-ray.
On CT scans, a network of more transparent areas (known as reticular opacities) can be seen, which is
due to lung destruction, honeycombing, fibrosis (see above), and bronchiectasis. CT scanning is an
advanced imaging technique that uses x-rays and computer technology to produce more clear and
detailed pictures than a traditional x-ray. Bronchiectasis is irreversible widening and destruction of the
walls of the bronchi. It is unclear if bronchiectasis is due to interstitial pneumonia or the frequent bacterial
infections that these patients often experience. These findings are present in almost all patients with UIP
and are usually found beneath the pleura and towards the bottom of both sides of the lungs. Remember,
the pleura is the smooth, moist double layer of flexible tissue that lines the lungs and the chest wall. UIP is
also known as idiopathic pulmonary fibrosis (IPF).
DESQUAMATIVE INTERSTITIAL PNEUMONIA (DIP): This type of interstitial pneumonia occurs in current
or past smokers. Current smokers are usually affected in the 30s or 40s and feel out of breath after only
mild physical exertion. Although this condition is called pneumonia, there is no evidence that the
inflammation is caused by an infection. The lesions in this type of pneumonia are spread throughout the
tissue and are usually the same size. There is mild inflammation in the interstitial tissue and fibrosis (see
last section) is present. There are many macrophages present in the alveoli (tiny air sacs) with a light
brown coloring. A macrophage is a type of white blood cell that eats bacteria. Hyperplasia of the lung
occurs, which means that there is an increased number of cells present.
Chest x-rays generally show less severe changes than in UIP (see above). For example, in this type of
pneumonia, there is little honeycombing. As much as 10% of patients with desquamative interstitial
pneumonia may have no changes on x-ray. Tests of lung functioning show a decrease in the amount of air
contained in the lungs at the end of a person’s best effort to take a breath. There is also a decreased
amount of oxygen in the blood.
LYMPHOID INTERSTITIAL PNEUMONIA (LIP): This is an uncommon lung disease in which mature
lymphocytes and plasma cells build up in the alveoli (see above) and in the spaces between alveoli. A
lymphocyte is a type of white blood cell present in the blood. Plasma is the watery part of blood.
LIP occurs in children, but rarely in adults. In children, LIP occurs in anywhere between 22 and 75% of
children with lung disease. About 25% of LIP cases occur in people with Sjogren’s syndrome. Sjogren's
(pronounced SHOW-grins) syndrome is a type of disease in which the eyes and mouth become
excessively dry.
LIP can also occur in children and adults with HIV infection (a type of sexually transmitted disease). Only
3% of adults with HIV-related lung disease have LIP. However, LIP is common in children with HIV. In fact,
the Centers for Disease Control and Prevention lists LIP as an illness that defines the progression of HIV
into AIDS (Acquired Immune Deficiency Syndrome) in children. AIDS is a decrease in the effectiveness of
the body's immune (defense) system that is due to infection from HIV.
In patients who do not have HIV, LIP is more common in women. LIP progresses slowly and leads to the
formation of cysts in the lungs. A cyst is an abnormal lump, swelling, or sac that contains fluid, a part solid
material, or a gas, and is covered with a membrane. A membrane is a thin layer of flexible tissue that
covers something.
Pulmonary fibrosis can be a long-term complication of patients with LIP and often develops slowly.
Respiratory distress has been reported, especially in children with LIP. Lymphoma can also result from
lymphoid interstitial pneumonia. Lymphoma is cancer of the lymphatic tissue. The lymphatic system is a
system of vessels that drain lymph from all over the body and back into the blood. Lymph is a milky fluid
that contains proteins, fats, and white blood cells (which help the body fight off diseases).
A condition known as pseudolymphoma is a variant of LIP that causes the build-up of harmless abnormal
tissue masses. Pseudolymphoma is not a disease, but is an inflammatory reaction to certain known or
unknown stimuli.
ACUTE INTERSTITIAL PNEUMONIA (AIP): AIP is a type of interstitial pneumonia that comes on suddenly
(acute) and with great severity. It has no known cause. AIP is also known as severe interstitial lung
disease, idiopathic adult respiratory distress syndrome, and Hamman-Rich Disease.
CRYPTOGENIC INTERSTITIAL PNEUMONIA (CIP): CIP is a type of interstitial pneumonia with the
following characteristics. First is the presence of polyps that contain granulation tissue in the tubular
space of bronchioles (the smallest airways of the lungs) and alveolar ducts. The alveolar ducts are part of
the airway passages that are positioned away from the bronchioles. Polyps are a type of growth that
projects from the lining of mucous membranes. A mucous membrane is one of four major types of thin
sheets of tissue that line or cover various parts of the body. Granulation tissue is a combination of new
connective tissue and tiny blood vessels.
The second characteristic of CIP is the presence of patchy areas of pneumonia, consisting largely of
mononuclear cells and foamy macrophages (a type of white blood cell that eats bacteria). Mononuclear
cells are cells with one nucleus. A nucleus is the structure at the center of a cell. CIP is also known as
cryptogenic organizing pneumonia and bronchiolitis obliterans organizing pneumonia (BOOP).
RESPIRATORY BRONCHIOLITIS-ASSOCIATED INTERSTITIAL LUNG DISEASE (RB-ILD): RB-ILD is a
mild type of interstitial lung disease seen in heavy cigarette smokers. Symptoms include cough, phlegm
production, and uncomfortable breathing. Two thirds of patients have crackles that can be heard when the
doctor taps the chest area and listen for sounds. Pulmonary function tests show a restrictive defect. After
the patient stops smoking, damage in the lungs seen on CT scan appears to remain stable or resolve
slowly without progressing to lung disease with fibrosis.
NONSPECIFIC INTERSTITIAL PNEUMONIA (NSIP): NSIP is a type of interstitial pneumonia that cannot
be classified into one of the above types. This is why it is called “nonspecific.” NSIP may share features
of several of the above types of interstitial pneumonia. NSIP begins somewhat quickly.
WHAT ARE THE SIGNS AND SYMPTOMS OF INTERSTITIAL PNEUMONIA?
The signs and symptoms of interstitial pneumonia include progressively worse discomfort while breathing,
fever, occasional wheezing, blue discoloration of the skin, and an abnormal enlargement of the end of the
fingers (known as clubbing). There also tends to be a non-productive cough for one to three years. The
term “non-productive” means that no phlegm is brought up when the person coughs. When the doctor
listens to the lung sounds while breathing, he/she can hear a crackling noise on the bottom of both sides
of the lungs.
For people with lymphoid interstitial pneumonia (LIP), enlargement of lymph nodes or lymph vessels may
occur. Lymph nodes are small egg shaped structures in the body that help fight against infection. Lymph
vessels are tube-shaped structures that carry lymph throughout the body. Lymph is a milky fluid that
contains proteins, fats, and white blood cells (which help the body fight off diseases).
People with LIP may also experience enlargement of the liver, spleen, and parotid glands. The spleen is
an organ next to the stomach that helps fight infection and removes and destroys worn-out red blood cells.
The parotid gland is the largest of three pairs of glands that produce saliva. Enlargement of these glands
is present in about 33% of adult patients.
WHAT CAUSES INTERSTITIAL PNEUMONIA?
Causes of interstitial pneumonia include infection with a bacteria known as Pneumocystis carinii, inhaling
poisons, and radiation exposure. Radiation is a type of energy in the form of waves or streams of
particles. Radiation is often used to treat cancer which is any of a large group of malignant diseases
characterized by an abnormal, uncontrolled growth of new cells in one of the body organs or tissues.
Interstitial pneumonia can be a rare complication of measles. Measles is a viral illness that leads to a
fever and a characteristic rash. Some other forms of pneumonia, such as viral pneumonia, can lead to
interstitial pneumonia. Viral pneumonia is pneumonia that is caused by a virus. In lymphoid interstitial
pneumonia, what seems to happen is that there is an increased production of lymphocytes in responses
to the presence of viruses in the body.
Individual viruses or combinations of viruses may be responsible for interstitial pneumonia. Some types of
viruses that may be responsible for lymphoid interstitial pneumonia include HIV, the Epstein-Barr virus,
and human T-cell leukemia virus (HTLV) type 1. Traces of these viruses have been found in individuals
with interstitial pneumonia. Epstein-Barr virus is one of the most common viruses in the world.
HTLV is a virus that causes T-cell leukemia. Leukemia is a type of cancer in the blood in which bone
marrow (a tissue that fills the openings of bones) is replaced by early forms of white blood cells. In T-cell
leukemia, the T-cells (types of white blood cells) are malignant, meaning that these cells grow in an
abnormal and uncontrolled way.
Hypersensitive reactions to certain medications can lead to interstitial pneumonia. Some of these
medications include the anti-cancer drugs Methotrexate, Busulfan, and Chlorambucil, as well as the blood
pressure medication, Hexamethonium.
Interstitial pneumonia can also be an autoimmune reaction, meaning that the body’s defense system
attacks the body by mistake. The reason why interstitial pneumonia is thought to be possibly an
autoimmune reaction is because it often accompanies other autoimmune disorders (see the next section).
In fact, about 30% of people with interstitial pneumonia have autoimmune disorders.
With regards to a genetic component, patients with allele types named “HLA-DR5” and “HLA-DR6” are
predisposed to developing a diffuse visceral lymphocytosis syndrome with lymphoid interstitial pneumonia.
An allele is a form of a gene. Genes are units of material contained in a person's cells that contain coded
instructions as for how certain bodily characteristics (such as eye color) will develop. Diffuse visceral
lymphocytosis syndrome is a condition in which lymphocytes infiltrate salivary gland, tear glands, lung
tissue, kidney tissue, stomach tissue, intestinal tissue, and breast tissue. The salivary glands are the
glands in the mouth that produce saliva. A gland is an organ in the body made of special cells that form
and release materials such as fluid.
WHAT OTHER DISORDERS ARE ASSOCIATED WITH INTERSTITIAL PNEUMONIA?
As was mentioned in the last section, autoimmune disorders such as Sjogren’s syndrome (see above),
celiac sprue, rheumatoid arthritis, and progressive systemic sclerosis are associated with interstitial
pneumonia. Celiac sprue is an uncommon, long-term disorder, in which the lining of the small intestine
wastes away, becomes inflamed, and is damaged by a protein known as gluten. This protein is found in
wheat, rye, barley, and other cereals. The intestine is a tube shaped structure that is part of the digestive
tract. It stretches from an opening in the stomach to the anus (rear end) and occupies most of the lower
parts of the belly. The small intestine is a part of the intestine that takes in all of the nutrients that the body
needs.
Rheumatoid arthritis is a disorder in which the body's defense system attacks its own tissues, causing
inflammation of bone joints. A joint is a place where two bones contact each other. Progressive systemic
sclerosis is a rare condition in which the body mistakenly attacks many organs and tissues of the body.
Too much collagen builds up in people with progressive systemic sclerosis. Collagen is a protein found in
the skin. As a result of the collagen build up, the skin becomes thick and tight.
Lymphoid interstitial pneumonia (LIP) is associated with HIV, a type of sexually transmitted disease. LIP
is also associated with human T-cell leukemia virus (HTLV) type 1, (see last section). The association of
LIP, HIV, and HTLV seems to be common in people with African ancestry. Of note is that LIP appears to
cluster is southwestern Japan, where HTLV is common.
Lymphoid interstitial pneumonia is associated with other conditions such as lymphoma, Hashimoto
thyroiditis, myasthenia gravis, pernicious anemia, autoerythrocyte sensitization syndrome, chronic active
hepatitis, common variable immunodeficiency, and allogenic bone marrow transplantation. These
conditions are described below.
Lymphoma is cancer of the lymphatic tissue. Lymphatic tissue is a network of fibers and cells that contain
various degrees of lymphocytes (types of white blood cells). Hashimoto thyroiditis is a disease in which
the immune system attacks and destroys the thyroid gland. The thyroid gland is a butterfly-shaped organ
located in the front of the neck that plays an important role in metabolism. Metabolism is the chemical
actions in cells that release energy from nutrients or use energy to create other substances.
Myasthenia gravis is a type of disorder in which the muscles get weak and tire easily as a result of poor
conduction (transmission) of nerve impulses. Anemia is a condition in which there is an abnormally low
amount of hemoglobin in the blood. Hemoglobin is substance present in red blood cells that help carry
oxygen to cells in the body. Vitamin B12 is necessary for the formation of red blood cells. Pernicious
anemia is a type of anemia caused by a lack of intrinsic factor, which is a substance needed to absorb
vitamin B12 from the digestive tract.
Autoerythrocyte sensitization syndrome is a rare bruising disorder that mostly affects people with severe
emotional disturbance. Chronic active hepatitis is continuing inflammation of the liver. The liver is the
largest organ in the body and is responsible for filtering (removing) harmful chemical substances,
producing important chemicals for the body, and other important functions.
Common variable immunodeficiency is a disorder characterized by low levels of antibodies in the blood
and an increased susceptibility to infections. Antibodies are types of proteins that are formed by the body
to destroy foreign proteins known as antigens. Allogenic bone marrow transplantation is an operation that
replaces affected bone-marrow with a healthy one taken from donor. Bone marrow is a type of tissue that
fills the inside of bones.
DOES INTERSTITIAL PNEUMONIA BEGIN SLOWLY OR QUICKLY?
Interstitial pneumonia begins slowly and for this reason, the condition often goes untreated for many
months. In fact, many patients are mistakenly treated for other diseases instead. Because of this problem,
breathing ability can be significantly deteriorated by the time the condition is diagnosed.
IS THERE A DIFFERENCE IN THE NUMBERS OF MEN AND WOMEN THAT DEVELOP INTERSTITIAL
PNEUMONIA?
Men have a slightly higher rate of developing interstitial pneumonia. Approximately 29 per 100,000 men
develop interstitial pneumonia whereas 26 out of 100,000 women develop it.
DO PEOPLE WITH INTERSTITIAL PNEUMONIA HAVE HIGHER RATES OF CANCER?
Yes, people with interstitial pneumonia have higher rates of cancer that begins in the bronchi of the lungs.
HOW IS INTERSTITIAL PNEUMONIA DIAGNOSED?
Tests of lung functioning are used as part of the diagnostic approach to interstitial pneumonia. These tests
show a decrease in the amount of air contained in the lungs at the end of a person’s best effort to take a
breath. There is also a decreased amount of oxygen in the blood. Lung functioning tests can also detect
impaired diffusion capacity, which is the ability of the lungs to transfer gases across the alveoli.
Obstructive airway disease is found in some patients. Obstructive airway disease is a disease
characterized by decreased airway size and increased secretions into the airways. A secretion is a
substance that is formed and released
X-rays of the lungs are also used diagnose interstitial pneumonia combined with knowledge of the
patient’s medical history. X-rays of the lungs of patients with interstitial pneumonia will show patchy
shadows and blotchy areas. In early stages, a hazy appearance of ground glass is present in the lungs.
The ground glass appearance is common in DIP and RB-ILD.
The lung tissue will have an abnormal, honeycombed appearance, much like a bee hive. This happens in
about one third of the cases. The honeycombs are actually holes in the lung that are about 1 centimeter
wide. The presence of honeycombs usually represents the end stage of many forms of lung disease.
Honeycombing is especially common in UIP.
As was mentioned earlier, some patients with late-stage interstitial pneumonia have a pneumothorax that
is noticeable on x-ray. A pneumothorax is the presence of air or gas in the pleural space, causing a lung
to collapse. The pleural space is a thin, fluid-filled opening between the pleura of the lungs and the pleura
of the chest wall. The pleura is the smooth, moist double layer of flexible tissue that lines the lungs and the
chest wall. The pleura often appears thickened in interstitial pneumonia. Pleural effusions (see earlier
section) can also be seen on x-ray. It is worth noting that X-rays appear normal in about 16% patients
with interstitial pneumonia.
Computerized tomography (CT) scans are also used to help diagnose interstitial pneumonia, detect the
extent of disease, and to follow disease progression. CT scanning is an advanced imaging technique that
uses x-rays and computer technology to produce more clear and detailed pictures than a traditional x-ray.
CT scans can show the widening and destruction of the walls of the bronchi. In active disease, the hazy
appearance of ground glass can also be seen. The tissue between the alveoli can appear thickened and
distorted.
On CT scans, a network of more transparent areas (known as reticular opacities) can be seen, which is
due to lung destruction, honeycombing, and fibrosis (an overgrowth of connective tissue), and
bronchiectasis. Bronchiectasis is irreversible widening and destruction of the walls of the bronchi. A
similar, widespread, net-like pattern can sometimes be seen on X-rays. Many of the abnormal findings on
X-rays and CT scans are found beneath the pleura and towards the bottom of both sides of the lungs.
A technique known as a brochoalveolar lavage (BAL) is sometimes performed, in which a viewing device
is placed into one of the bronchi (airways connected to the lungs), salt water is injected into the end of the
airway and about 50 to 70% of it is then sucked out by hand. The saltwater is then sent to the laboratory
for analysis. The laboratory analysis helps diagnose which bacteria are causing the infection.
The laboratory analysis often finds monocytosis or lymphocytosis. Monocytosis is an increased number of
monocytes, which are large oval shaped white blood cells. White blood cells are cells that help the body
fight off infections. Lymphocytosis is an increased number of lymphocytes. Lymphocytes are another type
of white blood cell.
Lab values can also be helpful in diagnosing lymphoid interstitial pneumonia. For example, in children with
LIP and HIV, levels of the lactate dehydrogenase (LDH) are 300-500 International Units per liter (normal
level is about 105-333 IU/L). LDH is an enzyme found in many body tissues and organs. An enzyme is a
type of protein that helps produce chemical reactions in the body. Injury to organs and tissues often cause
a release of LDH into the blood, which raises the level of this enzyme on blood tests. Lactate
dehydrogenase levels are not helpful measures in adults when trying to diagnose interstitial pneumonia.
An International Unit is very similar to a unit but is based on a different type of scale. The value of an
International Unit will also differ for each type of substance. A liter is a measurement of the amount of
space that a liquid takes up in a container, which is equal to 1.056688 quarts. To understand this better,
picture a gallon of milk. It takes 4 quarts of milk to make up one gallon of milk. Since one liter is a little bit
more than one quart, 4 liters of milk is a little bit more than one gallon of milk.
Another common laboratory finding in LIP is hypergammaglobulinemia. Hypergammaglobulinemia is an
abnormal increase in gamma globulins found in the blood, often in chronic infections diseases. Gamma
globulins are globulins (large, globe-shaped proteins) that move to an area known as the gamma region
upon electrophoresis.
Electrophoresis is the movement of charged molecules, such as proteins, in an electric field.
Electrophoresis produces a graph-like pattern that doctors can examine. One of the areas on the graph is
known as the gamma region. Antibodies are types of gamma globulins that are increased on
electrophoresis.
A biopsy of the lungs is often needed to diagnose desquamative interstitial pneumonia (see above),
especially when other findings cannot lead to a diagnosis. A biopsy is the process of removing living
tissue or cells from organs or other body parts of patients for examination under a microscope or in a
culture to help make a diagnosis, follow the course of a disease, or estimate a prognosis. A culture is an
artificial way to grow cells or tissues in the laboratory.
The biopsy technique used to collect lung tissue specimens is known as a transbronchial lung biopsy. If
multiple biopsies are taken from several affected areas of the lungs, this procedure can generally lead to a
definitive diagnosis. This biopsy procedure is usually done by a doctor who specializes in the lungs
(known as a pulmonologist) or a thoracic surgeon. A thoracic surgeon is a doctor that specializes in
surgery of diseases of the chest. If a transbronchial lung biopsy is performed, x-rays are done afterwards
to be sure that the patient does not have a post-operative pneumothorax or that if one is present, it is
small and stable A pneumothorax is the presence of air or gas in the pleural space, causing a lung to
collapse.
In desquamative interstitial pneumonia, the biopsy usually shows a distinctive pattern of widespread and
evenly distributed lung inflammation. The most striking feature of the lung biopsy is the presence of
numerous macrophages in the alveoli and bronchioles (smallest airways). A macrophage is a type of white
blood cell that eats bacteria. Macrophages normally help get rid of bacteria and small particles in the
alveoli.
It is important to note that patients with rheumatoid arthritis and progressive systemic sclerosis can have
identical laboratory findings as patients with interstitial pneumonia, making it important for the doctor to
consider other clinical factors (such as history and symptoms) when making the diagnosis. See above for
a description of rheumatoid arthritis and progressive systemic sclerosis.
HOW IS INTERSTITIAL PNEUMONIA TREATED?
Medications are used to treat patients that show symptoms of disease or whose physical functioning is
affected. The doctor should weigh the risks and benefits of medication treatment with the patient. A
commonly used medication for interstitial pneumonia is corticosteroids. Corticosteroids (such as
Prednisone) are a group of drugs that act similarly to a natural chemical in the body known as
corticosteroid hormone. Corticosteroid hormones control the body's use of nutrients and the amount of
water and salts in the urine. These drugs are used in interstitial pneumonia because they help decrease
inflammation.
Corticosteroids are effective in about 10 to 15% of patients with interstitial pneumonia, but cause serious
complications in about 26% of individuals. The doctor will decide the best dose of corticosteroids for the
patient’s condition and may decrease the dose after a month of treatment.
Patients with UIP and AIP tend to respond poorly to corticosteroids whereas patients with RB-ILD, NSIP,
and DIP tend to respond well to corticosteroids. Those who tend to respond well to corticosteroids tend to
be young women, those with active inflammation on lung biopsy, and those with a ground glass
appearance on CT scans of the chest. See the last section for more information on biopsies and CT scan
results.
Some physicians use cytotoxic drugs, in combination with corticosteroids, to treat interstitial pneumonia.
Cytotoxic dugs, such as Cytoxan and Azathioprine, are drugs that kill certain cells in the body.
Medications that widen the bronchi (known as bronchodilators) are used to treat wheezing.
For patients who do not respond to high doses of corticostreroids, alkylating medications (a type of anti-
cancer drug) are sometimes used. Only doctors that are experienced with the usage and side effects of
this type of medication should prescribe these drugs. When prescribed, alkylating medications are usually
given for weeks at a time. The progression of the disease and complete blood count (CBC) tests need to
be monitored when taking this type of medication. The CBC test shows the number of various types of red
and white blood cells. The way in which alkylating medications treat interstitial pneumonia is unclear.
Treatment of interstitial pneumonia can last many months and usually involves bed rest and oxygen
therapy. Oxygen supplements may be needed if lab findings indicate decreased oxygen levels. Physical
activity may need to be reduced if the patient is experiencing decreased oxygen levels. However, on an
outpatient basis, depending on the patient’s condition, the doctor may prescribe an exercise course such
as walking a long corridor or several flights of steps.
It is important for patients to monitor changes in their saliva or phlegm as this may be the only sign of
infection. Associated lung infections will be treated with antibiotics. Progression of the disease can be
monitored by follow-up CT scans. It is worth noting that patients with LIP who do not have symptoms and
whose physical functioning is not affected may not require treatment.
WHAT IS THE PROGNOSIS FOR PEOPLE WITH INTERSTITIAL PNEUMONIA?
The prognosis for people with interstitial pneumonia varies based on the type of disease they have.
However, in general terms the prognosis is poor, with 87% of patients dying from causes related to this
condition. Most patients with interstitial pneumonia die within 6 months to a few years because of lung or
heart failure. The average length of survival is four to six years. In general, the prognosis of patients with
interstitial pneumonia is better when patients are on a combination of therapies. Patients with acute
interstitial pneumonia may die quickly even with supportive therapy.
For patients with usual interstitial pneumonia (see above), recovery is not possible. About 45% of people
with UIP live past 5 years and only 10% respond to treatment. About 68% of people with UIP eventually
die from this condition. Similarly, about 62% of patients with AIP die from that condition. The average
person with AIP only lives for only 1 to 2 months.
For patients with LIP, the prognosis is variable, with a disease duration between 1 month and 11 years.
LIP is often stable for months without treatment and sometimes improves spontaneously. It is common
however for symptoms to recur.
For patients with LIP who do not have HIV infection, half improve with treatment, but relapse is common.
Despite treatment, end stage fibrosis may occur. Fibrosis is the production of firm connective tissue (scar
tissue). In the past, high death rates were reported in older patients with LIP, but death rates in patients
with LIP are inexact due to the lack of follow-up studies. It is noteworthy that patients with LIP and HIV
have better survival rates and a slower decline in CD4 T-cells (types of white blood cells) than patients
with LIP but not HIV.
The situation is much better for patients with desquamative interstitial pneumonia, in which about 70% of
patients live for 10 years or more. In fact, the average person with DIP lives for 12 years. About 27% of
people with DIP die from this condition. The prognosis for people with DIP improves when they quit
smoking and start taking corticosteroids (see last section).
About 11% of people with NSIP die from this condition, with the average length of survival being 17
months. The situation is best for people with RB-ILD, as it is rare for people to die from this mild condition.
WHAT ELSE IS INTERSTITAL PNEUMONIA KNOWN AS?
Interstitial pneumonia is also known as giant cell pneumonia, giant cell interstitial pneumonia, Hecht
pneumonia, diffuse fibrosing pneumonia, alveolitis, and Hamman-Rich syndrome.
WHAT IS THE ORIGIN OF THE TERM, INTERSTITIAL PNEUMONIA?
Interstitial pneumonia comes from the Latin word “inter” meaning “between,” the Latin word “sistere”
meaning “to stand,” and the Greek word “pneumon” meaning “lung.” Put the words together and you have
“to stand between lung.”