


MedFriendly®
"Where Medical Information is Easy to Understand"™

Chondromalacia patellae is a painful disorder of the knee in which the cartilage directly behind the kneecap (also known as the patella) becomes soft and damaged. Cartilage is a type of tissue that helps form many important body structures. The type of cartilage affected in chondromalacia patellae is called articular cartilage. The word "articular" means "referring to a joint." A joint is a place where two bones contact each other. The knee is an example of a joint. Thus, since the cartilage affected in chondromalacia patellae is located directly behind a joint, it is called articular cartilage.
WHO USUALLY GETS CHONDROMALACIA PATELLAE?
Chondromalacia patellae usually happens to young adults after a knee injury. It is particularly common in teenagers and is more common in females. Chondromalacia patellae rarely occurs in older adults (ages 40 and older). When it does, it is known as retropatellar arthritis. People with a history of trauma to the knee such as a break or dislocation, are more likely to get this condition. A dislocation in when any body part (usually a joint) is out of its normal position. Someone can have a partial dislocation (partly out of the normal position) or a complete dislocation (completely out of the normal position).
WHO USUALLY GETS CHONDROMALACIA PATELLAE?
Chondromalacia patellae usually happens to young adults after a knee injury. It is particularly common in teenagers and is more common in females. Chondromalacia patellae rarely occurs in older adults (ages 40 and older). When it does, it is known as retropatellar arthritis. People with a history of trauma to the knee such as a break or dislocation, are more likely to get this condition. A dislocation in when any body part (usually a joint) is out of its normal position. Someone can have a partial dislocation (partly out of the normal position) or a complete dislocation (completely out of the normal position).

Chondromalacia Patallae
WHAT ARE THE SIGNS AND SYMPTOMS OF CHONDROMALACIA PATELLAE?
The signs and symptoms of chondromalacia patellae include sensitivity and pain around the kneecap, swelling, and wearing away of the knee cartilage. Sensitivity is usually felt in the lower, inside part of the knee. The pain is usually felt in the front of the knee. However, the pain may radiate to the back of the knee. The pain comes and goes, but usually happens when the knee is straightened and is usually very bad when using stairs. Other situations that make the knee pain worse is sitting, kneeling, squatting, running, cycling, or exercising for a long period of time. Squatting or deep knee bends causes increased pressure between the kneecap and the femur, which can put one at risk for chondromalacia patellae.
The knee may feel stiff or may buckle when the leg is moved. The knee may appear mildly swollen when the doctor examines it. In addition, the kneecap may not line up with the femur below. The femur is the long bone of the leg that runs from the hip to the knee.
When the leg is straightened out, pressing the kneecap against the femur may cause pain. If the knee is flexed from a bent position, a grinding sensation may be felt below the kneecap. This may be accompanied by a clicking sound. The wearing away of the knee cartilage can be seen on pictures of the knee taken with an x-ray.
WHAT CAUSES CHONDROMALACIA PATELLAE?
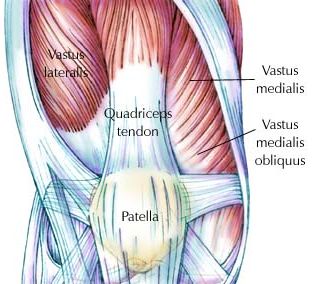
Causes of chondromalacia patellae include trauma to the knee (such as a fracture or bruise) and abnormal forces acting upon the knee. Another cause of chondromalacia patellae is overusing the knee in the performance of activities in which the knee is bent more than it is straight (such as exercising beyond one's tolerance). An example of such an activity would be bike riding. Trauma to the knee or overuse of the knee can weaken the inner part of the quadriceps muscle. The quadriceps muscle is a muscle with four distinct parts that is responsible for straightening the knee. The quadriceps and the kneecap are pictured to the right:
The signs and symptoms of chondromalacia patellae include sensitivity and pain around the kneecap, swelling, and wearing away of the knee cartilage. Sensitivity is usually felt in the lower, inside part of the knee. The pain is usually felt in the front of the knee. However, the pain may radiate to the back of the knee. The pain comes and goes, but usually happens when the knee is straightened and is usually very bad when using stairs. Other situations that make the knee pain worse is sitting, kneeling, squatting, running, cycling, or exercising for a long period of time. Squatting or deep knee bends causes increased pressure between the kneecap and the femur, which can put one at risk for chondromalacia patellae.
The knee may feel stiff or may buckle when the leg is moved. The knee may appear mildly swollen when the doctor examines it. In addition, the kneecap may not line up with the femur below. The femur is the long bone of the leg that runs from the hip to the knee.
When the leg is straightened out, pressing the kneecap against the femur may cause pain. If the knee is flexed from a bent position, a grinding sensation may be felt below the kneecap. This may be accompanied by a clicking sound. The wearing away of the knee cartilage can be seen on pictures of the knee taken with an x-ray.
WHAT CAUSES CHONDROMALACIA PATELLAE?
Causes of chondromalacia patellae include trauma to the knee (such as a fracture or bruise) and abnormal forces acting upon the knee. Another cause of chondromalacia patellae is overusing the knee in the performance of activities in which the knee is bent more than it is straight (such as exercising beyond one's tolerance). An example of such an activity would be bike riding. Trauma to the knee or overuse of the knee can weaken the inner part of the quadriceps muscle. The quadriceps muscle is a muscle with four distinct parts that is responsible for straightening the knee. The quadriceps and the kneecap are pictured to the right:

If the quadriceps muscle becomes weakened, it is less able to do its job and straighten out the knee. As a result, the knee will become tilted when an attempt is made to straighten it. The tilting of the kneecap will cause it to rub unevenly against the lower end of the femur (the long bone of the leg that runs from the hip to the knee). This rubbing action can become excessive and may soften, roughen, and break down the smooth and shiny cartilage under the kneecap. Normally, the kneecap runs smoothly across the lower end of the femur. Many adolescents with chondromalacia patellae have a mild misalignment of the kneecap.
In teenagers, the above factors may combine with rapid growth and natural changes in the structure of the legs to cause damage to the cartilage. In periods of rapid growth, especially in girls, any natural inward curving of the legs that causes the knees to touch and the feet to be farther apart is made worse. This puts extra pressure on the outer part of the kneecap, causing the cartilage under the kneecap to break down. Outward rotation of the lower leg in relation to the femur can also lead to chondromalacia patellae.
Extra and uneven pressure on the kneecap can also be caused by imbalance between two parts of the quadriceps muscle. Remember that the quadriceps muscle is a muscle with four distinct parts that is responsible for straightening the knee. Two of these parts, known as the vastus lateralis and vastus medialis can become imbalanced. As you can see in the pictured to the right, the vastus lateralis is to the side of the knee and the vastus medialis is in the middle area.
The vastus lateralis is usually stronger than the vastus medialis in people with chondromalacia patellae. This increases the chance for the kneecap to be pulled to the side. Pulling of the kneecap to the side puts it at an abnormal angle, places extra pressure on the side of the knee, and causes it to weaken the cartilage.
In people over age 40, chondromalacia patellae usually occurs as part of the wear and tear process that affects the rest of the body through normal aging. In older people, one of the first places where the cartilage will break down is behind the kneecap.
In teenagers, the above factors may combine with rapid growth and natural changes in the structure of the legs to cause damage to the cartilage. In periods of rapid growth, especially in girls, any natural inward curving of the legs that causes the knees to touch and the feet to be farther apart is made worse. This puts extra pressure on the outer part of the kneecap, causing the cartilage under the kneecap to break down. Outward rotation of the lower leg in relation to the femur can also lead to chondromalacia patellae.
Extra and uneven pressure on the kneecap can also be caused by imbalance between two parts of the quadriceps muscle. Remember that the quadriceps muscle is a muscle with four distinct parts that is responsible for straightening the knee. Two of these parts, known as the vastus lateralis and vastus medialis can become imbalanced. As you can see in the pictured to the right, the vastus lateralis is to the side of the knee and the vastus medialis is in the middle area.
The vastus lateralis is usually stronger than the vastus medialis in people with chondromalacia patellae. This increases the chance for the kneecap to be pulled to the side. Pulling of the kneecap to the side puts it at an abnormal angle, places extra pressure on the side of the knee, and causes it to weaken the cartilage.
In people over age 40, chondromalacia patellae usually occurs as part of the wear and tear process that affects the rest of the body through normal aging. In older people, one of the first places where the cartilage will break down is behind the kneecap.
HOW IS CHONDROMALACIA PATELLAE DIAGNOSED?
Chondromalacia patellae is diagnosed by a doctor, who will do a physical examination and will try to make sense of the symptoms described and his own personal observations. The frequency in which the signs and symptoms occur will also be important. The doctor will likely send the patient for an x-ray of the knee to see if the pictures show a wearing away of the knee cartilage or if the knee cap is abnormally tilted to the side. In many cases, however, the x-ray is normal.
In the early stage of knee pain, there may not be any actual breakdown in the cartilage. In such a case, the condition is not chondromalacia patellae. A better name for frontal knee pain without cartilage damage would be anterior (frontal) knee pain syndrome. It should be mentioned that many teenagers have frontal knee pain, on and off for several years, which eventually goes away permanently once growth is complete.
Chondromalacia patellae is diagnosed by a doctor, who will do a physical examination and will try to make sense of the symptoms described and his own personal observations. The frequency in which the signs and symptoms occur will also be important. The doctor will likely send the patient for an x-ray of the knee to see if the pictures show a wearing away of the knee cartilage or if the knee cap is abnormally tilted to the side. In many cases, however, the x-ray is normal.
In the early stage of knee pain, there may not be any actual breakdown in the cartilage. In such a case, the condition is not chondromalacia patellae. A better name for frontal knee pain without cartilage damage would be anterior (frontal) knee pain syndrome. It should be mentioned that many teenagers have frontal knee pain, on and off for several years, which eventually goes away permanently once growth is complete.
HOW IS CHONDROMALACIA PATELLAE TREATED?
Initially, chondromalacia patellae is usually treated with rest and painkillers. This often helps to decrease the sensitivity and pain in the knee. The painkillers are usually over-the-counter medications that decrease inflammation, known as non-steroidal anti-inflammatories (abbreviated as NSAIDs). An example of such a medication is Motrin. Doctors generally have patients take the painkiller regularly, whether they are in pain or not. Painkillers help to reduce inflammation, which decreases the pain. There is also some evidence that NSAIDs help reform the damaged cartilage.
Exercise, physical therapy, and electrical stimulation are used to decrease the pressure between the kneecap and the femur and to strengthen and stretch the inner part of the quadriceps muscle (see above) and hamstrings. Hamstrings are a group of muscles at the back of the thigh that bend the knee and swing the leg backwards from the thigh. This form of treatment usually fixes the problem. A description of these exercises is listed below. However, keep in mind that exercises that increase knee pain should be avoided until the pain improves (through rest, for example). Participation is strenuous physical activity, such as sports, should also be avoided.
Initially, chondromalacia patellae is usually treated with rest and painkillers. This often helps to decrease the sensitivity and pain in the knee. The painkillers are usually over-the-counter medications that decrease inflammation, known as non-steroidal anti-inflammatories (abbreviated as NSAIDs). An example of such a medication is Motrin. Doctors generally have patients take the painkiller regularly, whether they are in pain or not. Painkillers help to reduce inflammation, which decreases the pain. There is also some evidence that NSAIDs help reform the damaged cartilage.
Exercise, physical therapy, and electrical stimulation are used to decrease the pressure between the kneecap and the femur and to strengthen and stretch the inner part of the quadriceps muscle (see above) and hamstrings. Hamstrings are a group of muscles at the back of the thigh that bend the knee and swing the leg backwards from the thigh. This form of treatment usually fixes the problem. A description of these exercises is listed below. However, keep in mind that exercises that increase knee pain should be avoided until the pain improves (through rest, for example). Participation is strenuous physical activity, such as sports, should also be avoided.
For teenagers, the goal of the exercises is to restore the normal position of the kneecap. This is done by strengthening the vastus medialis obliquus, a muscle that stabilizes the kneecap. Once the kneecap is steady and muscle balance is restored, the pain improves. For teenagers that want to stay active in sports, a knee brace is typically recommended so that the kneecap remains stable. The type of knee brace that is typically used is called a patella stabilizing brace. Also, arch supports inside the sneakers can help runners keep their legs aligned.
If the pain continues after this form of treatment, it may mean that damage has been done to the cartilage. If this is the case, surgery may be needed. The goal of the surgery is to permanently change the angle of the kneecap so that the cartilage does not rub against the bone of the leg. The surgical procedure used is called arthroscopic surgery. Arthroscopic surgery is surgery that involves using a flexible viewing tube (known as an endoscope) to view a joint, such as the knee. The endoscope is inserted through tiny incisions in the skin and a light pain-numbing medication is used. This helps prevent the big scars that occur from a regular surgery in which big cuts are needed to slice the skin open.
In the surgery mentioned above, the doctor will used the endoscope to make sure that the knee is tracking abnormally to the side. To correct this, the vastus lateralis muscle is divided from the inside. The vastus lateralis muscle is located to the side of the knee and can be seen above. Dividing the vastus lateralis muscle helps weaken it. Thus, it cannot pull the kneecap to the side as it did prior to the surgery because balance is restored to the quadriceps muscle. The quadriceps muscle is a muscle with four distinct parts that is responsible for straightening the knee. After this surgery, physical therapy is used for 6 weeks to bring the knee back to health and so the patient can return to sports.
For some people, even after intense physical therapy and surgery, the pain continues. This usually happens in patients in which there are severe problems with the structure of the knee. For example, the kneecap can be dislocated. In such severe cases, extensive restructuring of the quadriceps muscle and/or kneecap may be needed. In rare cases, the kneecap needs to be removed. Surprisingly, such a surgery does not limit one's movements much.
WHAT IS THE PROGNOSIS FOR PEOPLE WITH CHONDROMALACIA PATELLAE?
Chondromalacia patellae usually gets better on its own but it can persist for years. Overall, when non-surgical treatment is used (such as exercise and electrical stimulation) about 85% of patients improve to the point that no further treatment is needed. For people that need surgery, about 90% improve. About 15% of patients develop pain severe pain and/or the condition becomes worse enough for surgery to be required. In younger people, the condition usually resolves through a combination of exercise, physical therapy, and electrical stimulation (see previous section). In older people (over age 40), the condition generally gets worse over time. It can eventually progress to osteoarthritis of the knee. Osteoarthritis is a disease of the joints that is made worse by physical stress (e.g., aging, wear and tear).
CAN CHONDROMALACIA PATELLAE BE PREVENTED?
Whether or not someone will develop chondromalacia patellae largely depends on the structure of the knee and muscle imbalance around the knee. If the person is tall, thin, and has knees that touch with feet wide apart, he/she is more likely to develop the condition. Small kneecaps or tightness of the muscles to the side of the quadriceps (see above) also make one more likely to develop chondromalacia patellae.
Although some of the above factors are beyond the person's control, there are some things that can be done to decrease the chance of developing the condition. One thing to do is to warm-up and stretch the muscles (especially the quadriceps and hamstrings) out before exercising. Hamstrings are a group of muscles at the back of the thigh that bend the knee and swing the leg backwards from the thigh. The goal is to keep the hamstring muscles strong and flexible. Avoiding trauma, abnormal stress, and repetitive pressure on the knee is also helpful for prevention. Avoiding obesity is also helpful. Obesity is an abnormal increase in the amount of fat cells in the body compared to the amount of other types of cells.
Exercise and sporting activities can be varied to decrease the chance of developing chondromalacia patellae. For example, instead of running every day, one can run one day and do swimming the next day. Or instead of running, one can do gentle jogging. There are also some exercises that can be done to decrease the chances of developing this condition. These exercises can also help decrease frontal knee pain, but it usually takes 6 weeks to see improvement. Doctors typically recommend that these exercises be done twice a day. These exercises are listed below:
One exercise is to use a stationary exercise bike (a bike that stays in one place while riding it) because it does not put much stress on the knee (as opposed to running). The trick here is to adjust the seat on the bike high enough so that the leg is straight on the down stroke. This exercise is typically done for 15 minutes at first, with the goal of eventually doing it for 30 minutes a day.
Another exercise involves lying down on the back and lifting one leg in the air for 5 seconds. Then the leg is lowered to the ground slowly. While doing this, the other leg is relaxed. Yet another exercise involves sitting up with the legs extended. The quadriceps muscles are tightened and the knees are pushed to the ground for 5 seconds. The next exercise involves lying on the back with a rolled up towel under the thigh. The leg and foot should be kept in the air for 5 seconds. The foot is then lowered as the knee is bent slowly.
Another exercise that people have found helpful for chondromalcia patellae is to hang the legs over the edge of the bed and to raise the lower part of the leg so the knee is straight. The goal for all of the exercises above is 10 times for each leg that is causing pain, two times a day. Another exercise that can be done involves hanging the leg over the side of the bed and swinging it gently. This last exercise is done for two minutes (for each leg causing pain).
The last exercise involves sitting on a chair and straightening the leg(s) with the heel(s) resting on the ground. For this exercise, both hands are rested on the knee. Then, the hands are moved forwards towards the toes until tightness or slight pain is felt in the hamstrings. Once tension (for example, tightness or slight pain) is felt, the position is held for 10 seconds and relaxed. This last exercise is usually repeated 20 times with both legs and is done 3 times a day over a time period of three weeks.
The further you can move the hands towards the toes, while keeping the legs extended straight, the more stretched the hamstrings are. Be sure to consult a doctor to see if the exercises mentioned above are right for you.
WHAT IS THE DIFFERENCE BETWEEN CHONDROMALACIA PATELLAE AND PATELLOFEMORAL ARTHRALGIA?
Patellofemoral arthralgia is pain in the front of the knee. In most cases of patellofemoral arthralgia, the articular cartilage is not injured as it is in chondromalacia patellae. There is little evidence that untreated patellofemoral arthralgia leads to chondromalacia patellae.
WHAT IS THE ORIGIN OF THE TERM, CHONDROMALACIA PATELLAE?
Chondromalacia patellae comes from the Greek word "chondros" meaning "cartilage," the Greek word "malakia" meaning "softness," and the Latin word "patella" meaning "small dish" (referring to the kneecap). Put the words together and you have "small dish cartilage softness."
If the pain continues after this form of treatment, it may mean that damage has been done to the cartilage. If this is the case, surgery may be needed. The goal of the surgery is to permanently change the angle of the kneecap so that the cartilage does not rub against the bone of the leg. The surgical procedure used is called arthroscopic surgery. Arthroscopic surgery is surgery that involves using a flexible viewing tube (known as an endoscope) to view a joint, such as the knee. The endoscope is inserted through tiny incisions in the skin and a light pain-numbing medication is used. This helps prevent the big scars that occur from a regular surgery in which big cuts are needed to slice the skin open.
In the surgery mentioned above, the doctor will used the endoscope to make sure that the knee is tracking abnormally to the side. To correct this, the vastus lateralis muscle is divided from the inside. The vastus lateralis muscle is located to the side of the knee and can be seen above. Dividing the vastus lateralis muscle helps weaken it. Thus, it cannot pull the kneecap to the side as it did prior to the surgery because balance is restored to the quadriceps muscle. The quadriceps muscle is a muscle with four distinct parts that is responsible for straightening the knee. After this surgery, physical therapy is used for 6 weeks to bring the knee back to health and so the patient can return to sports.
For some people, even after intense physical therapy and surgery, the pain continues. This usually happens in patients in which there are severe problems with the structure of the knee. For example, the kneecap can be dislocated. In such severe cases, extensive restructuring of the quadriceps muscle and/or kneecap may be needed. In rare cases, the kneecap needs to be removed. Surprisingly, such a surgery does not limit one's movements much.
WHAT IS THE PROGNOSIS FOR PEOPLE WITH CHONDROMALACIA PATELLAE?
Chondromalacia patellae usually gets better on its own but it can persist for years. Overall, when non-surgical treatment is used (such as exercise and electrical stimulation) about 85% of patients improve to the point that no further treatment is needed. For people that need surgery, about 90% improve. About 15% of patients develop pain severe pain and/or the condition becomes worse enough for surgery to be required. In younger people, the condition usually resolves through a combination of exercise, physical therapy, and electrical stimulation (see previous section). In older people (over age 40), the condition generally gets worse over time. It can eventually progress to osteoarthritis of the knee. Osteoarthritis is a disease of the joints that is made worse by physical stress (e.g., aging, wear and tear).
CAN CHONDROMALACIA PATELLAE BE PREVENTED?
Whether or not someone will develop chondromalacia patellae largely depends on the structure of the knee and muscle imbalance around the knee. If the person is tall, thin, and has knees that touch with feet wide apart, he/she is more likely to develop the condition. Small kneecaps or tightness of the muscles to the side of the quadriceps (see above) also make one more likely to develop chondromalacia patellae.
Although some of the above factors are beyond the person's control, there are some things that can be done to decrease the chance of developing the condition. One thing to do is to warm-up and stretch the muscles (especially the quadriceps and hamstrings) out before exercising. Hamstrings are a group of muscles at the back of the thigh that bend the knee and swing the leg backwards from the thigh. The goal is to keep the hamstring muscles strong and flexible. Avoiding trauma, abnormal stress, and repetitive pressure on the knee is also helpful for prevention. Avoiding obesity is also helpful. Obesity is an abnormal increase in the amount of fat cells in the body compared to the amount of other types of cells.
Exercise and sporting activities can be varied to decrease the chance of developing chondromalacia patellae. For example, instead of running every day, one can run one day and do swimming the next day. Or instead of running, one can do gentle jogging. There are also some exercises that can be done to decrease the chances of developing this condition. These exercises can also help decrease frontal knee pain, but it usually takes 6 weeks to see improvement. Doctors typically recommend that these exercises be done twice a day. These exercises are listed below:
One exercise is to use a stationary exercise bike (a bike that stays in one place while riding it) because it does not put much stress on the knee (as opposed to running). The trick here is to adjust the seat on the bike high enough so that the leg is straight on the down stroke. This exercise is typically done for 15 minutes at first, with the goal of eventually doing it for 30 minutes a day.
Another exercise involves lying down on the back and lifting one leg in the air for 5 seconds. Then the leg is lowered to the ground slowly. While doing this, the other leg is relaxed. Yet another exercise involves sitting up with the legs extended. The quadriceps muscles are tightened and the knees are pushed to the ground for 5 seconds. The next exercise involves lying on the back with a rolled up towel under the thigh. The leg and foot should be kept in the air for 5 seconds. The foot is then lowered as the knee is bent slowly.
Another exercise that people have found helpful for chondromalcia patellae is to hang the legs over the edge of the bed and to raise the lower part of the leg so the knee is straight. The goal for all of the exercises above is 10 times for each leg that is causing pain, two times a day. Another exercise that can be done involves hanging the leg over the side of the bed and swinging it gently. This last exercise is done for two minutes (for each leg causing pain).
The last exercise involves sitting on a chair and straightening the leg(s) with the heel(s) resting on the ground. For this exercise, both hands are rested on the knee. Then, the hands are moved forwards towards the toes until tightness or slight pain is felt in the hamstrings. Once tension (for example, tightness or slight pain) is felt, the position is held for 10 seconds and relaxed. This last exercise is usually repeated 20 times with both legs and is done 3 times a day over a time period of three weeks.
The further you can move the hands towards the toes, while keeping the legs extended straight, the more stretched the hamstrings are. Be sure to consult a doctor to see if the exercises mentioned above are right for you.
WHAT IS THE DIFFERENCE BETWEEN CHONDROMALACIA PATELLAE AND PATELLOFEMORAL ARTHRALGIA?
Patellofemoral arthralgia is pain in the front of the knee. In most cases of patellofemoral arthralgia, the articular cartilage is not injured as it is in chondromalacia patellae. There is little evidence that untreated patellofemoral arthralgia leads to chondromalacia patellae.
WHAT IS THE ORIGIN OF THE TERM, CHONDROMALACIA PATELLAE?
Chondromalacia patellae comes from the Greek word "chondros" meaning "cartilage," the Greek word "malakia" meaning "softness," and the Latin word "patella" meaning "small dish" (referring to the kneecap). Put the words together and you have "small dish cartilage softness."
