MedFriendly®
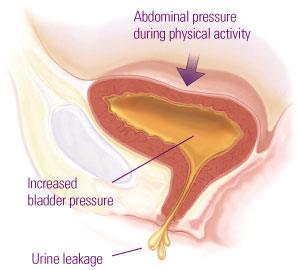
Stress incontinence is the most common form of urinary incontinence
(involuntary or uncontrollable urine loss). It occurs when a physical
movement or activity increases pressure inside the abdomen, which
places involuntary pressure on the urinary bladder. Examples of such
physical activities include coughing, laughing, lifting, exercising,
sneezing, bending over, running, lifting, straining, intercourse, and
even standing.
The more vigorous and straining the physical activity, the more likely it
is to cause stress incontinence. The leakage will not necessarily
occur after every instance of physical activity. Each person differs in
terms of which physical activities cause stress incontinence and how
often.
Increased physical pressure on
the bladder from the abdomen
causes leakage of urine.
The leakage amount from stress incontinence can be just a drop, multiple drops, a squirt, or a stream.
The term ďstressĒ in stress incontinence refers to physical pressure on the bladder, not emotional stress.
Being emotionally stressed, in and of itself, does not cause stress incontinence. However, if one were
crying profusely due to emotional stress and straining the abdominal area then this could be an activity
that could trigger urine leakage, although it is not the underlying cause.
HOW IS STRESS INCONTINENCE DIFFERENT FROM URGE INCONTINENCE?
Stress incontinence is due to a physical movement or activity whereas urge incontinence (overactive
bladder) is the involuntary loss of urine for no apparent reason (although the urinary bladder is
contracting), usually while feeling a sudden urge to urinate. In stress incontinence, the bladder may not
feel unusually full. Mixed urinary incontinence, which is a combination of stress and urge incontinence.
WHAT CAUSES STRESS INCONTINENCE?
As noted above, stress incontinence occurs when a physical movement or activity increases pressure
inside the abdomen, which places involuntary pressure on the urinary bladder. Stress incontinence is
also caused by decreased strength and functioning of the bladder control muscles that regulate the
release of urine. This muscle is the urethral sphincter. A sphincter is a muscle that forms a circle around
a tube, natural opening, or duct in the body. The urethral sphincter controls the passage of urine from
the urinary bladder to the urethra. The urethra is a tube shaped structure that drains urine from the
bladder so it can leave the body.
The urethra and bladder are supported by pelvic floor muscles. If support from those muscles are weak
and insufficient (the most common cause of stress incontinence), the urethra can move down when
pressure inside the abdomen increases, allowing urine to pass through when pressure is placed on the
abdomen. If the pelvic floor muscles do not contract quickly enough or with enough force, urine leakage
may occur because the urethra will not seal shut. The bladder can also drop down into a position that
prevents the urethra from closing completely, resulting in urine leakage.
There is an external and internal urethral sphincter. External sphincters are under voluntary control
because they are made of skeletal muscle. Internal sphincters are made of smooth muscle, which are
not under voluntary control. Along with surrounding pelvic floor muscles, the urinary sphincter supports
the bladder. If the urethral sphincters do not work properly, this can cause stress incontinence. A
hypermobile urethra is a more common cause of stress incontinence than dysfunction of the internal
urethral sphincter.
Pregnancy and childbirth are the most common causes of stress incontinence in women. It is estimated
that about 1 in 5 women over age 40 have some degree of stress incontinence. For women who have
stress incontinence, the urethral sphincter and pelvic floor muscles may lose strength due to those
areas being stretched in pregnancy and childbirth. This is because the process of delivering a child can
damage nerves and tissues important for urinary bladder control. Stress incontinence can present soon
after childbirth or years later. A delay in the pushing phase of labor, forceps delivery, and multiple
vaginal deliveries are associated with higher rates of later developing stress incontinence. In women
with pelvic prolapse, in which the bladder, urethra, and rectum wall stick out through the vagina, stress
incontinence is common.
Another factor that can contribute to stress incontinence (immediately or delayed) is a hysterectomy
(surgical removal of the uterus) or other surgeries in the pelvic area because it can alter the functioning
and support of the bladder and urethra. The uterus is a hollow organ in a female's body where the egg
is implanted and the baby develops. Physical changes from menopause can also cause stress
incontinence. Menopause is the time in a woman's life when periods no longer occur. A period (also
known as menstruation) is the shedding of the lining of the uterus that generally occurs once every 28
days in women who are not pregnant. However, physical changes to the body caused by menstruation
can lead to stress incontinence.
For men who have stress incontinence, the urethral sphincter and pelvic floor muscles may lose
strength due to surgical removal of the prostate gland after treating prostate cancer. This is the most
common cause of stress incontinence in men. The prostate gland is an organ near the bladder that
produces a reproductive fluid. The prostate gland lies directly above the urethral sphincter and
encircles the urethra. As a result, due to the close proximity, surgery to the prostate can weaken the
urethral sphincter and result in less urethral support. Radiation treatment of prostate cancer can also
contribute to stress incontinence. Other causes of stress incontinence include injury to the urethra area,
inflammation of the prostate gland, medications, and chronic urinary tract infections.
WHAT FACTORS CAN WORSEN STRESS INCONTINENCE?
Stress incontinence is more likely to happen when the bladder is full. Stress incontinence can be made
much worse by being overweight or obese. This is because excess weight puts pressure on the
abdominal and pelvic organs, which then pressures the bladder, even without added pressure from a
cough or force. Other factors that can worsen stress incontinence are illnesses/conditions that cause
chronic coughing and/or sneezing, smoking (because it can cause frequent coughing), high impact
activities over many years, and excessive consumption of alcohol or caffeine. Getting older is also a
risk factor for stress incontinence because the muscles become weaker. However, stress incontinence
is not a normal part of aging. Medications that increase urine production can lead to stress
incontinence. Urinary tract infections can also worsen stress incontinence.
For women, stress incontinence can worsen in the week before the menstrual period. This is because
low estrogen levels during that time can lead to lower muscle pressure around the urethra, which
increases the chance of urine leakage. Estrogen is a type of hormone that promotes the growth of
some physical female sexual characteristics. Hormones are natural chemicals produced by the body
and released into the blood that have a specific effect on tissues in the body. Low estrogen levels can
also contribute to stress incontinence due to menopause. High level female athletes may also
experience stress incontinence when participating in sports (e.g., tennis, running) that involve abrupt
repeated increases in pressure within the abdomen. This pressure exceeds resistance pressure from
the pelvic floor.
Diabetes mellitus can make stress incontinence worse because it results in excess urine production
and can cause nerve damage. Diabetes mellitus is a medical condition in which the body is not able to
effectively use a natural chemical called insulin. Insulin's main job is to quickly absorb glucose (a type
of sugar) from the blood into cells for their energy needs and into the fat and liver (a large organ that
performs many chemical tasks) cells for storage.
IS STRESS INCONTINENCE MORE COMMON IN WOMEN THAN MEN?
Yes, stress incontinence is twice as common in women as in men. It is also the most common type of
urinary incontinence in women. Stress incontinence is rare in men.
WHAT ARE PSYCHOLOGICAL EFFECTS OF STRESS INCONTINENCE?
People with stress incontinence may feel embarrassed, distressed, isolate themselves, and restrict
their activities (e.g., work, social life, leisure activities, and exercise). Embarrassment is common if
urinary incontinence accidents occur and if a person needs to wear absorbent pads or incontinence
garments. Stress incontinence can interfere with work, social activities, and interpersonal relationships
(including intimacy).
HOW IS STRESS INCONTINENCE DIAGNOSED?
Initially, the doctor will perform an interview and review the medical records to understand the medical
history. A physical exam will be performed that focuses on the abdominal, pelvic, rectal, and genital
area. This allows for the strength of the pelvis to be assessed by contracting and relaxing certain
muscle groups. A brief neurological exam may be performed to identify problems with nerves in the
pelvis and to identify sensory problems. Strength, sensation, and reflexes in the legs may also be
assessed. In some women, the pelvic exam may show that the bladder or urethra is bulging into the
genital area (known as a cystocele). The doctor will likely also perform a urinary stress test when the
bladder is full, in which the doctor will ask the patient to stand and then will observe if any urine is lost
when coughing, bearing down, changing positions, or bouncing on the heel(s). A catheter may be put in
place during this test.
Another diagnostic test is called the pad test, in which the patient is asked to exercise while wearing a
sanitary pad. The pad is weighed after exercise to see how much urine has been lost. The doctor may
also request that the patient keep a urinary diary, which records fluid intake, the number of times a
person urinated during the day and night, and how many times a urine leaking occurred. A health care
provider may request that the diary be kept for 3 to 5 days.
Tests such as a urine analysis, cystometry (also known as a cystometrogram), and postvoid residual
are usually normal. The urine test checks for signs of infection, blood traces, sugar levels, or other
abnormalities. Cystometry is a diagnostic test that evaluates bladder functioning by using a catheter
(thin hollow tube) to fill the bladder slowly with warm water. This tests the personís perception of water
filling the bladder, urgency to urinate, involuntary bladder contractions, and bladder filling capacity.
Testing for bladder leakage is done during the filling phase to check for stress incontinence. This can
be combined with a pressure-flow study which tells how much pressure is needed for the bladder to
empty completely. Cystometry is often done with people who have spinal cord damage/disease. The
postvoid residual test measures the amount of urine left in the bladder within 15 minutes after urinating.
This can be done by asking the patient to urinate and then checking the bladder contents afterwards
with an ultrasound. Ultrasound scanning is a procedure that uses high-frequency sound waves to
produce images of internal body structures. Typically, an ultrasound of the abdomen and/or pelvis is
what is ordered. Another way to do this test is to use a catheter to drain the remaining urine from the
bladder. Post-void residual studies are usually combined with cystometry to tell whether the urinary
sphincter exerts enough pressure to keep the urethra closed as bladder pressure increases. These
techniques can indentify abnormal voiding patterns or urine blockages.
Another test that may be used to evaluate stress incontinence is cystoscopy. This involves inserting a
scope into the bladder to evaluate the bladder and urethra. Another diagnostic method is known as
video urodynamics (or uroflowmetry), which creates pictures of the bladder as it is filling and emptying.
This technique works by giving the patient a warm fluid mixed with dye via a cathether. The colored
fluid gradually shows up on x-ray or ultrasound images as the bladder is recorded. The recording
continues as the fluid enters and leaves the body. The doctor may also order x-rays of the kidneys. The
kidneys are two organs located on each side of the spine, behind the stomach that filter (remove)
wastes from the blood. Video urodynamics is often combined with cystometry. Rarely, an
electromyogram (EMG) is ordered to study muscle activity in the urethra or pelvic floor. An EMG
measures electrical impulses to assess the health and strength of muscles and the nerves that control
muscles.
In addition to an ultrasound, other tests that can be used to evaluate structural abnormalities of the
urinary tract are computerized axial tomography scanning (CT scanning) and an intravenous pyelogram
(IVP). CT scanning is an advanced imaging technique that uses x-rays and computer technology to
produce more clear and detailed pictures than a traditional x-ray. An IVP is a technique in which x-rays
are used to take pictures of the urinary tract, after a liquid substance called contrast is injected into a
vein (a blood vessel that caries blood to the heart).
HOW IS STRESS INCONTIENCE TREATED?
Treatment of stress incontinence is helpful to improve oneís overall sense of well-being. The treatment
selected depends on how bad the symptoms are and how much they are affecting daily life. A
combination of treatments is typically used. The good news is that stress incontinence can often be
cured.
BEHAVIORAL TREATMENTS:
Behavioral treatments are simple, self-directed, have no side effects, and can be used when combined
with other treatments. The first behavioral treatment typically recommended is exercise that
strengthens the pelvic floor muscles, urinary sphincter, bowels, and uterus, to keep them working
properly. These exercises are known as pelvic floor exercises or Kegel exercises. About 60% of stress
incontinence cases can be cured with this method. Some research has shown that these exercises
should be the treatment of choice for stress incontinence although other research indicates that the
sling surgical procedure should be offered as an initial treatment because it is more effective than
Kegel exercises. See the surgery section below for a discussion of the sling technique.
Kegel exercises involve tightening the pelvic floor muscles as hard as possible by pretending that one
is trying to stop the urine stream or trying not to pass gas. Kegel exercises work best in women under
age 60. Each contraction is held for a slow count of 5 seconds followed by relaxing the contraction.
These are called slow-ups. When performing the contractions quickly for a second or two and
repeated at least five times, these are referred to as fast pull-ups.
Kegel exercises must be performed regularly to control urine leakage, which means at least 24
contractions a day for six weeks. Others suggest doing 50 contractions a day and others suggest
repeating five slow pull-ups and five fast pull-ups for five minutes at least 3 to 10 times a day,
alternating between sitting, standing, and lying down. As the muscles become stronger, the length of
time each slow pull-up is held can be increased up to 10 seconds. After several weeks, the muscles
will start to feel stronger and the contractions can be held for longer periods without feeling tired.
Some advocate performing the exercises for at least 3 months and note that it often takes 8 to 20
weeks for most improvement to occur and for a cure to occur. To stop the problem from recurring,
Kegel exercises can be performed as a part of everyday life (1 to 2 five-minute sets a day).
When performing the exercises, it is advised to try and not move the leg, abdominal muscles,
buttocks, or abdomen muscles. Only the pelvic muscles should be squeezed. When these exercises
are performed properly, no one should be able to tell that they are being done but the patient will feel
some movement in the muscle. Kegel exercises can initially be performed while sitting on the toilet or
chair with the knees kept slightly apart. They can also be done when standing or lying down. Once
Kegel exercises are learned they can be performed anywhere during everyday life. When done
effectively, Kegel exercises can prevent the urge to urinate. The key to preventing urine leakage is to
contract the pelvic muscles just in time to squeeze the urethra closed. Performing the contraction just
in time is known as the knack.
Healthy lifestyle changes are sometimes used to treat stress incontinence. An example is weight loss
because it relieves pressure on the bladder and pelvic floor muscles. Losing about 5 to 10 percent of
body weight can help improve stress incontinence. When weight loss is combined with exercise and a
restrictive diet, it can reduce stress incontinence episodes by as much as 70%. If possible, not
running or jumping as much can decrease stress incontinence as can decreasing other activities
known to cause stress incontinence.
Quitting smoking can help treat stress incontinence because it irritates the bladder and causes
coughing, which puts stress on the bladder. Treating a chronic cough caused by reasons other than
smoking can also help treat stress incontinence. Smoking also decreases oxygen carrying capacity,
which is thought to increase the risk of an overactive bladder.
Scheduled toilet trips can help for patients with mixed incontinence because this helps decrease the
number and severity of urge incontinence episodes. Specifically, urinating more frequently will reduce
the amount of urine that leaks because less of it will be available. It is also helpful to choose seating
that is close to the bathroom. By keeping a journal to determine when leaking occurs, going to the
bathroom at those times can help avoid leakage. It should be as easy as possible to get to the toilet,
which may require using handrails or a raised seat if the toilet is difficult to access.
Another strategy for treating stress incontinence is bladder training, in which someone slowly
increases the time intervals between urinating (e.g., every 30 minutes, then 45 minutes, then 60
minutes, etc.,) until one can go three to four hours without leaking between urination episodes. Some
people try another technique in which they do not go to the bathroom for 15 minutes after the first
urge. This is done for two weeks until the interval is increased slowly (e.g., 20 minutes, 25 minutes, 30
minutes, etc.).
Decreasing the amount of fluid consumed throughout the day and the times that fluids are consumed
throughout the day can also help in managing stress incontinence. Avoiding beverages with caffeine
(e.g., coffee, soda), tea (regular or decaffeinated), and alcohol may be necessary because these
drinks can stimulate and irritate the bladder. Keep in mind that not drinking enough fluid can lead to a
concentration of waste in the urine which can irritate the bladder. Other foods that can be avoided due
to causing bladder irritation include spicy foods, citrus foods, and carbonated beverages. Adding fiber
(e.g., fruits, vegetables, whole grains) to the diet (or use of laxatives) can help treat urinary
incontinence if chronic constipation is a contributing factor. The strain from constipation can worsen
urinary incontinence. Dietary fiber helps keep bowel movements soft and regular, which allows urine
to flow freely and decreases the strain on the pelvic floor muscles. Keeping blood sugar under control
in people who have diabetes mellitus can reduce stress incontinence.
There is a medical device known as a perineometer which measures the strength of voluntary pelvic
floor muscle contractions. Some women use a vaginal cone with Kegel exercises, which is discussed
in the medical device section below.
MEDICATIONS:
One way to treat stress incontinence is through medications, although medications are usually more
helpful for people with urge incontinence. When medications help with stress incontinence, it tends to
be in people with mild to moderate forms of the problem. When treating patients with medications who
have stress incontinence, most health care providers prescribe anti-muscaranic drugs, which are
medications that block bladder contractions. There are also anti-cholinergic drugs that are used,
which help control an overactive bladder by calming the bladder contractions. Examples of anti-
cholinergic medications include: oxybutynin (Ditropan, Oxytrol), tolterodine (Detrol), darifenacin
(Enablex), trospium chloride (Sanctura), and solifenacin succinate (Vesicare). Estrogen creams with
progesterone can reduce symptoms os stress incontinence.
Alpha-adrenergic agonists are sometimes used to treat stress incontinence. These are medications
that stimulate alpha-1 adrenergic receptors. These receptors help contract the neck of the urinary
bladder and urethra. By stimulating these receptors, these agonists make the smooth muscle stronger
in the urethral sphincter and help close the internal sphincter. Examples of these types of medications
include clonidine (Catapres), ephedrine, phenylpropanolamine, and pseudoephedrine. Although these
medications can be used with people who have mild stress incontinence not caused by nerve
damage, the evidence for their effectiveness is weak and they tend to be avoided due to significant
side effects including insomnia, agitation, anxiety (although Clonidine is often used to treat anxiety),
and heart problems. This is why people with heart disease or high blood pressure should not take
these medications. They also should not be used in people who have glaucoma, diabetes mellitus, or
hyperthyroidism. Glaucoma is a condition in which increased pressure in the eye can lead to gradual
loss of vision. Hyperthyroidism is a condition in which the thyroid gland is overactive. The thyroid
gland is a butterfly-shaped organ located in front of the neck that produces a natural chemical known
as hormones that affect virtually every cell in the body and many functions such as disease fighting,
heart rate, energy level, and skin condition.
Because there is some evidence that stress incontinence may be partly caused by problems with
chemical messengers in the brain that are known to affect mood but also the normal action of urinary
bladder muscles and pathways/nerves involved in urination, some have treated stress incontinence
with antidepressant medications that affect the levels of these chemicals in the brain. These chemical
messengers include serotonin and norepinephrine (also known as noradrenaline). One group of
antidperessants is known as tricyclics, which are named after the three rings (three cycles) of
interconnected atoms that make up their structure. An example of such a medication is imipramine
(Tofranil), which blocks the chemical messenger, acetylcholine. This relaxes the bladder and makes
the internal sphincter stronger. However, tricyclics must be used carefully because they can cause
drowsiness, may cause harmful effects to the heart and lungs, overflow incontinence, and can have
more severe effects in the elderly. Overflow incontinence is the involuntary release of urine from an
overly full urinary bladder, usually in the absence of an urge to urinate.
A better anti-depressant option for most people is SNRIís (serotonin-norepinephrine reuptake
inhibitors) because they work similar to tricyclics without the same side effects. These medications
are so-named because they prevent the reuptake of serotonin and norepinephrine, leaving more of it
available in the brain. This stimulates the nerve that controls the urethral sphincter, allowing it to
contract more strongly. An example of an SNRI is duloxetine (Cymbalta), which is approved in Europe
(but not the U.S.) for stress urinary incontinence. One study showed that 60% of women who used
this medication had half the number of leakage incidents compared to before using the medication.
These medications are not likely to cure stress incontinence but can decrease the problem, especially
when combined with Kegel exercises. However, medication is an option for women who do not want
to have surgery or who are not good candidates for surgery.
Although low estrogen levels have been found to contribute to urinary incontinence, estrogen
replacement therapy (pill or skin patch form) has not been shown to be an effective treatment for
stress incontinence in women.
DEVICES:
Some people use moisture barriers, towels (preferably disposable), external catheters for men,
incontinence garments, and/or absorbent pads for women to treat stress incontinence. These
products are small and it is helpful to carry extras of them in a purse or backpack in case they are
needed along with an extra pair of clothes (e.g., in the trunk of a car, in a work office). Another device
is a urethral insert or plug, which is a small, disposable, tampon-like device inserted into the urethra to
prevent leakage. Although it can be worn throughout the day, they were not meant to be worn all day
and are usually worn to prevent leakage in specific situations.
Another device is a vaginal pessary, which is a ring-shaped object with two bumps that sit on each
side of the urethra. The pessary pushes the urethra against the symphysis pubis (a joint located
between the left and right pubic bones) and lifts the neck of the bladder. By supporting the bladder in
this way, the pessary keeps the urethra in its normal location and prevents urine leakage during
movement, especially if the bladder dropped. These are fitted and implanted by a doctor or nurse.
This is a good treatment option for people who want to avoid surgery but the device requires regular
removal for cleaning because it can cause vaginal discharge and vaginal/urinary tract infections.
Pesssaries and plugs help support the uterus, bladder, urethra, and rectum.
Another device used to treat stress incontinence in women is the vaginal cone (also known as a
vaginal weight). This small plastic device is designed and shaped to exercise the pelvic floor muscles
to restore proper bladder functioning. It is often performed in conjunction with Kegel exercises. After
the device is inserted into the body, the woman contracts her muscles to keep the weight from falling
out. After the woman does this with the lightest weight, the weight is increased over time which further
strengthens the pelvic muscles. The cone can be worn for up to 15 minutes at a time, twice a day.
After 4 to 6 weeks of use. Most women have some improvement in their symptoms. As a rule of
thumb, most doctors recommend that devices should be used as a supplement to Kegel exercises but
not as a replacement.
BIOFEEDBACK AND ELECTRICAL STIMULATION:
Biofeedback is a technique in which body processes (such muscle tension) are made perceptible to
the senses in order to control them with the power of thought. Biofeedback can be used to treat
stress incontinence by using electronic devices or diaries to track when the bladder and urethral
muscles contract. By making the patient more aware of this information with measuring devices,
computer graphs, and noise signals, the person can gain better control over those muscles. It is
useful to get this audible feedback because the pelvic muscles that need to be controlled cannot be
seen. The feedback provided can also allow the therapist to individualize oneís exercise program.
Research has shown that biofeedback is important for treating stress incontinence.
Muscle strength and stabilization in the lower pelvis and urethra can be improved with small doses of
low-voltage electrical stimulation that are sent into nearby body parts through electrodes. The current
makes weak or inactive pelvic muscles contract, like a Kegel exercise. After feeling which muscles
are contracting, the patient may be able to learn how to contract these muscles him/herself. Electrical
stimulation can be performed at home (under the instruction of a health care provider) or at the health
care providerís office. Overactive muscles can be stabilized as a result of this electrical stimulation
and it can stimulate the contraction of muscles in the urethra.
Electrical stimulation works after inserting a tampon-like device into the vagina, which is connected to
a handheld adjustable device that allows the patient to increase the flow of current. The electrical
stimulation is not uncomfortable but is set to a comfortable tingle sensation. It can be performed at
home and may be covered by insurance.
Electrical stimulation treatment of stress incontinence usually lasts 20-minutes and can be performed
once every 4 days. One technique involves use of an electromagnetic chair to make the pelvic floor
muscles contract when the person is sitting. Electrical stimulation is not a universally recommended
form of treatment for stress incontinence because it is not a scientifically proven treatment.
Biofeedback and electrical stimulation can be helpful for women who have difficulty doing Kegel
exercises and can help the patient find the correct muscle group to work.
SURGERY:
Surgery is another treatment option but is usually only tried once the exact cause of stress
incontinence has been found and once other treatment options have failed. It tends to be reserved for
severe cases. Most surgeries are minimally invasive, performed on an outpatient basis, and can treat
the vast majority of stress incontinence cases. The main goal of surgery is generally to reposition the
bladder neck and urethra. Possible side effects of surgery include an inability to urinate and
worsened incontinence. Surgical approaches differ depending on whether the urethra is hypermobile
or if the internal urethral sphincter is dysfunctional. Some surgery supports or tightens the neck of the
bladder and other surgery improves closing of the urethral sphincter.
The most common surgical approach for stress incontinence in women is a sling procedure, which
has about an 85% to 91% effectiveness rate, which is why some suggest it as an initial treatment
option over Kegel exercises. For a discussion of Kegel exercises, see the behavioral treatments
section above. In the sling procedure, the surgeon uses either the personís own tissue (e.g.,
abdominal tissue), animal/donor tissue (usually from a cow or pig), or synthetic mesh material, to
create a ribbon-shaped sling or hammock that supports the urethra, replacing the weak pelvic floor
muscles. The sling is placed under the urethra through one small vaginal incision and two small
abdominal incisions. The sling goes around the bladder neck and is attached to the pubic bone.
Some patients have alleged long-term harm and suffering from the implanted mesh.
One common sling technique is the tension-free transvaginal tape (also known as tension free
vaginal tape) (TVT), which uses a type of plastic known as polypropylene for the mesh tape under
the urethra. This is a minimally invasive sling procedure that supports the urethra and bladder neck.
The less invasive form of the sling approach is as effective as more invasive approaches. However,
the TVT technique has been associated with complications including perforation of the bladder and
mesh erosion from 1 day to 7 days later.
Another sling procedure is known as the transobturator tape (TOT) or Monarc sling procedure. The
technique attempts to reduce urinary incontinence by providing support under the urethra. It is a
minimally invasive procedure that eliminates the use of a needle. Rather, it involves making three
small incisions in the groin and inserting mesh tape under the urethra. Another sling procedure is
known as the readjustable sling or readjustable mechanical external device (REMEEX). This involves
the standard mesh sling combined with stitches that are attached to an implanted tensioning device
that is permanently placed under the skin of the abdominal wall. The device can be accessed again
under local anesthesia, which allows the sling to be adjusted if incontinence reappears. There is
another sling procedure known as a mini-sling, which involved introducing 8-cm of mesh through the
internal obdurator muscle (a pelvic muscle) with a metallic device. The benefits of this sling
procedure are that no external sling cuts are needed, no incisions are needed except for the vaginal
incision, it has low complication rates, and it provides a 67 to 90% cure rate. Yet another procedure is
the single needleless sling, which is a single incision TOT procedure. Only one unique incision is
needed to implant it and no needle is needed. It provides 135% more surface area than the mini
sling. There is a male sling procedure that can be performed in certain men, which is easier than
placing an artificial urethral sphincter (see below). Sling procedures are rarely done in men but can
be effective in some cases.
Surgical procedures in which support is provided to the urethra are known as urethropexy. A rare
surgical approach is an inflatable artificial urethral sphincter, which is an implanted device most often
used to treat men (this is rarely done in women). This involves fitting a fluid-filled cuff around the top
part of the urethra to replace the function of the sphincter. The cuff is connected via a tube to a
balloon that regulates pressure in the pelvic region. In other words, the patient can open and close
the cuff to control leakage. In men, the cuff is also connected to a pump in the scrotum that is
operated by hand. In women, the device is also connected to the labia (part of the female genitalia).
The artificial sphincter can be deflated by pressing a valve implanted under the skin.
Another surgical technique is known as retropubic colposuspension, which is performed after an
abdominal incision or laparoscopy. A laparoscopy is a surgical procedure (done under general
anesthesia) in which a thin viewing instrument known as a laparoscope is inserted into the abdomen
through a small incision made by (or in) the belly-button. Retropubic colposuspension is a group of
surgical procedures that involves using sutures attached either to a ligament, pubic bone, muscle
tissue behind the pubic bone, or sling (the sling is used in severe cases) to lift and support tissues
near the neck of the bladder and top part of the urethra. This helps the person get control over the
urine flow. A ligament is a tough band of tissue that attaches to joint bones. This procedure is often
used in combination with other procedures in women with stress incontinence who have a bladder
that has dropped down.
Most stress incontinence in women results from the urethra dropping down. Surgery can help bring
the urethra to a more normal position. This can be done through a single incision after which a
catheter is inserted into the urethra. An incision is then made across the abdomen to expose the
bladder and separate it from the surrounding tissue. These procedures hold up the bladder and
compress the bottom of the bladder and top of the urethra, which also prevents leakage. Retropubic
colposuspension is also known as the Marshall-Marchetti-Krantz (MMK) procedure, retropubic
suspension, or bladder neck suspension surgery. About 65% of women who undergo this procedure
no longer have stress incontinence. A modification to this surgery is known as the Burch modification,
which involves placing the sutures at the neck of the bladder and tying them to the pectineal
ligament. This is a ligament that attaches to the pubic bone.
Another surgical technique is anterior vaginal repair (or paravaginal) repair, which is a surgical repair
procedure that is performed when the bladder bulges into the vaginal area. Anterior repair is done
through a vaginal surgical cut whereas paravaginal repair is done through a vaginal or abdominal
surgical cut.
Another type of surgical approach is injectable bulking agents. This involves injecting gels, synthetic
chemicals, or connective tissues (most commonly gluteraldehyde cross-linked collagen, which comes
from pigs), or other natural materials (e.g., fat) into tissues around the top part of the urethra, which
makes it thicker, improves the ability of the urethral sphincter to close, and creates resistance against
the flow of urine, which helps control urine leakage. One positive aspect of this approach is that it is
not as invasive or expensive as other surgical approaches, which is why it may be tried before other
surgical techniques. It is most effective for patients with a fixed urethra. However, the downside is
that it is not a permanent fix, requiring the need to repeat it over time (e.g., every few months).
WHAT ARE COMPLICATIONS OF SURGERY FOR STRESS INCONTINENCE?
Complications of surgery for stress incontinence are rare but includes the wearing away of materials
placed during surgery (e.g., sling, artificial sphincter), discharge from the genital area, unpleasant
odors, pain during intercourse, infections of the urinary tract, skin breakdown/sores for sitting in
position too long after surgery (in cases of severe stress incontinence), skin irritation in the genital
area, fistulas, and abscesses. Fistulas are abnormal passages between two internal organs or
between an internal organ and a body surface. An abscess is a well-defined collection of pus that has
escaped from blood vessels and has been deposited on tissues or in tissue surfaces. Keeping the
skin as dry as possible helps prevent skin breakdown.
CAN STRESS INCONTINENCE BE CURED?
Yes. Stress incontinence can be cured with surgery. Although behavioral changes, medication, and
pelvic floor exercises can improve stress incontinence symptoms, these treatments do not lead to
cures. Treatment is less successful if prior surgery did not work, if there are other urinary or genital
problems, and if conditions are present that make healing or surgery more difficult.
CAN STRESS INCONTINENCE BE PREVENTED?
Performing Kegel exercises, which were discussed in the treatment section, can help prevent stress
incontinence, especially if performed during and after pregnancy and later in life. Maintaining an
average weight for oneís height can also help.
ARE THERE SUPPORT GROUPS FOR PEOPLE WITH URINARY INCONTINENCE?
Yes. The most well-known such group is the National Association for Continence. The group helps
people meet who have had various types of treatments for stress incontinence. These people can
share their experiences with different treatments. It can also help in coping with the social isolation
and social embarrassment that is sometimes associated with this problem.

Stress Incontinence