MedFriendly®


Tardive Dyskinesia
Tardive dyskinesia (often abbreviated TD) is a complication of
the long-term use of antipsychotic medications that is
Antipsychotic medications (also known as neuroleptics) are used
to treat psychosis and are known for their calming effects.
Psychosis is a mental disorder characterize by an impaired
ability to understand reality. Antipsychotic medications are
sometimes given to patients to treat problems with the stomach
and intestines. The intestine is a tube shaped structure that is
part of the digestive tract.
FEATURED BOOK: Stahl's Essential Psychopharmacology
WHAT ARE COMMON SIGNS AND SYMPTOMS OF TARDIVE
DYSKINESIA?
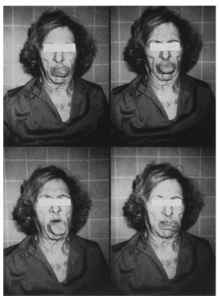
Tongue abnormalities
in tardive dyskinesia.
Common signs of TD include abnormal, involuntary, purposeless, and often repetitive
movements of the tongue and muscles of the face, jaw, arms, legs, and trunk. The trunk
refers to all the parts of the body, except the head, arms, and legs. The movements of
these body parts often appear rhythmic, writhing, or dance like. The movements of the
legs, arms, and trunk are often rapid. The most common sign of TD is known as orofacial
dyskinesia, which are abnormal movements of the mouth and face. These movements
may begin slowly and may start with mild tongue movements that progress to significant
movements with the lips and tongue. Examples of such abnormal movements include
sticking the tongue out, twitching of the tongue, bulging of the cheeks, arching of the
eyebrows, grimacing, smacking the lips together, licking the lips, puckering of the lips,
chewing movements, and sucking movements.
"Where Medical Information is Easy to Understand"™
Other signs of orofacial dyskinesia include continuous blinking of the
eyes, rapid eye blinking, and wrinkling of the eyebrows. Wiggling,
twisting, and tapping of the feet, hands, fingers, and toes are
common signs of TD. The patient's abnormal finger movements may
make it look like they are playing an invisible musical instrument like
the guitar or piano. Flexing and extending the ankles and toes is
also common. Abnormal ankle movements are also seen.
Other involuntary motor movements seen in TD may include rocking
back and forth, moving the head back or to the side, twisting,
swaying, writhing, flexing, jerking, and stiffening of almost any part
of the body, such as the neck.
Late appearing movements of the neck and truck are often referred to as "tardive dystonias." Rotation of
the hips is seen is some patients with TD.
Abnormal jerking movements can be present in the belly area and the diaphragm. The diaphragm is a
muscular-fibrous area that separates the chest and abdomen that assists in breathing. Abnormal
movements in the belly and diaphragm can make it difficult to breath, difficult to talk, and can cause
grunting sounds. The signs of TD can range from barely noticeable to severe. A symptom of TD includes
pain in the mouth and genitals (private parts).
IS THE PATIENT AWARE OF THE ABNORMAL MOVEMENTS CAUSED BY TARDIVE DYSKINESIA?
The patient is not always aware of the abnormal movements caused by TD. Family members and friends,
however, often alert the patient to the movements and make him/her more aware of it.
HOW IS TARDIVE DYSKINESIA DIAGNOSED?
To diagnose TD, the doctor will try to get a complete history from the patient and family member. The
doctor will determine how long the patient has been on the antipsychotic medications and what other
medications the patient has been on in the past. The doctor will try to determine when the signs of
possible TD began and how they have progressed.
The doctor will also try to rule out other possible causes of the movement problems. Once the doctor has
gathered all of the relevant information and has examined the patient, he/she will decide on the
appropriate diagnosis. The following general guidelines are used by doctors to support a diagnosis of TD
for patients under the age of 60 who have been taking an antipsychotic for at least 3 months: (For
patients, over 60, these guidelines apply if they have been taking antipsychotics for at least one month):
1) Development of at least 2 mild signs of TD, 2) Development of at least 1 moderate sign of TD, 3)
Development of at least 1 mild signs of TD within 4 weeks of discontinuing the antipsychotic, 4)
Development of at least 2 mild signs of TD within 8 weeks of discontinuing a depot neuroleptic, and 5)
Development of at least 1 moderate sign of TD within 8 weeks of discontinuing a depot neuroleptic. Depot
neuroleptics are an injected form of an antipsychotic drug that stays in the muscle and slowly releases
itself overtime.
Doctors often use rating scales to help them determine the presence and severity (for example, mild or
moderate) of TD. The most widely used rating scale is the Abnormal Involuntary Movement Scale (AIMS)
developed by the Psychopharmacology Research Branch of the National Institute of Mental Health. The
AIMS only takes a few minutes to administer. Doctors usually administer the AIMS before antipsychotics
are given so they can detect changes over time. The AIMS is usually administered every 3 months during
treatment with antipsychotics.
The abnormal movements of the trunk, jaw, tongue, arms, and legs typically need to last for at least 4
weeks in order to make a diagnosis of TD. The patient will also need to have been on the antipsychotics
for at least 3 months (or one month if over age 60). Many patients with TD are not able to keep their
tongue stuck out of the mouth for more than a second, so this is something the doctor will often assess.
The doctor will look to see if the abnormal movements are present while the person is resting, which is
what happens in TD. The abnormal movements should decrease when a particular body part is activated.
For example, placing the patient's fingers on his/her lips can stop abnormal movements of the lips.
Abnormal movements should increase when the patient is distracted. For example, asking the patient to
perform movements with the fingers may increase the abnormal movements in the tongue and face. The
abnormal movements caused by TD do not occur during sleep.
ARE THERE DIFFERENT CLASSIFCATIONS OF TARDIVE DYSKINESIA?
Yes. There are 6 basic classifications of TD:
1. PROBABLE TD: These are cases in which the patient has experienced at least moderate abnormal
involuntary movements (as determined by a rating scale) in one or more areas of the body or mild
abnormal involuntary movements in at least two or more areas of the body. To be diagnosed as probable
TD, the patient must be on antipsychotics for at least 3 months and other causes of abnormal involuntary
movements need to be ruled out.
2. MASKED PROBABLE TD: These are cases of probable TD (see above) in which the abnormal
movements go away when the dose of antipsychotics is increased or the antipsychotic is readministered
to the patient after it has been discontinued for some period of time.
3. TRANSIENT TD: These are cases in which the patient has had probable TD in the past, but upon
reexamination within 3 months, no longer have the abnormal movements when the dose of antipsychotics
is increased or when the antipsychotic is readministered to the patient after it has been discontinued for
some period of time.
4. PERSISTENT TD: These are cases in which the patient meets criteria for probable TD and continues
to do so for 3 months.
5. WITHDRAWAL TD: These are cases in which the patient develops significant abnormal involuntary
movements within 2 weeks after stopping the use of antipsychotic medications.
6. MASKED PERSISTENT TD: These are cases in which the patient meets criteria for probable TD, but in
which the abnormal involuntary movements disappear within 3 weeks of reintroducing or increasing the
dose of the antipsychotic to the patient after it has been discontinued for some period of time.
WHEN CAN TARDIVE DYSKINESIA OCCUR?
Tardive dyskinesia often occurs as a late side effect of some antipsychotic medications. It can occur as
early as three months, but is usually not observed until several years after taking antipsychotics. Some
patients develop TD when the antipsychotic is discontinued and others develop it when the dose of
antispsychotics is decreased. The abnormal movements seen in TD tend to be worse in the afternoon and
less in the morning.
WHAT CAUSES TARDIVE DYSKINESIA?
The causes of TD are not well understood and research continues to try and determine the answer to this
question. However, to understand the possible causes of TD, it is first necessary to understand how
antipsychotic medications work. Psychosis is caused by the presence of too much dopamine in the brain.
Dopamine is a chemical messenger in the brain that is important for slowing down movements, causing
pleasurable sensations, and other important functions.
Antipsychotic medications work by blocking dopamine receptors. Dopamine receptors are areas on nerve
cells that receive dopamine so that dopamine can exert its effect. There are different types of dopamine
receptors in the brain and each type is given a different number. For example, there is the dopamine-1
receptor, the dopamine-2 receptor, and the dopamine-3 receptor.
All antipsychotic medications block dopamine-2 receptors. When a nerve cell's dopamine receptors are
blocked, dopamine cannot exert its effect on that nerve cell. The overall effect of blocked dopamine
receptors is a decrease in the amount of dopamine stimulation in the brain. However, another result of
blocking dopamine receptors can be the signs and symptoms of tardive dyskinesia. This is the most
widely used explanation for why TD symptoms occur.
Specifically, the dopamine blockage hypothesis for TD is that the dopamine receptors that are not blocked
become oversensitive to the effects of dopamine, resulting in TD. The oversensitive dopamine receptors
are thought to be in the basal ganglia. The basal ganglia are paired groups of nerve cells located deep
within the brain that play an important part in sooth, continuous muscle movements and in starting and
stopping movements.
Many researchers believe that the blockage of dopamine receptors causes the brain to produce more
dopamine receptors in response. These extra dopamine receptors are believed to be oversensitive to
dopamine, even in low levels. The production of extra receptors is known as up-regulation.
Although the oversensitivity of dopamine receptors may explain the abnormal movements in TD for some
patients, research suggests that this hypothesis cannot fully explain TD. That is, there is some evidence
that oversensitive dopamine receptors contribute to the development of TD and there is other evidence to
argue against this explanation. For example, one research study found that there was no significant
increase in dopamine receptors in the brains of patients with TD, after they died. Also, some patients
develop oversensitivity to dopamine after a single dose but do not develop TD at that time. Rather, it
takes several months or years before patients develop TD.
Decreasing the sensitivity to dopamine does not always reduce the severity of TD. This has also led
others to criticize the hypothesis that oversensitive dopamine receptors lead to TD. What we know is that
there must be other explanations, in addition to oversensitivity to dopamine, for the cause of TD.
One important aspect to consider is which type of dopamine receptor is being blocked by the
antipsychotic medications. Most evidence shows that blockage of the dopamine-2 receptor is what
contributes to the development of TD. However, for some individuals, blockage of the dopamine-3,
dopamine-4, and dopamine-5 receptors may be involved in TD. Another consideration is where the
dopamine receptors are in the brain that are being blocked. Blocking dopamine areas in one part of the
brain will lead to overactive movements whereas blocking dopamine receptors in another area of the brain
can cause decreased movements.
Dopamine, however, may not be the only chemical messenger involved in TD, since research has
indicated that other chemical messengers such as serotonin, norepinephrine, and GABA (gamma-
aminobutyric acid) may also play a role. Some individuals may have inherited certain genes from their
parents that make it more likely to develop TD when exposed to certain drugs. Genes are tiny,
microscopic structures that contain coded instructions for how proteins should be constructed and how
certain bodily characteristics (such as eye color) should develop.
CAN MEDICATIONS BESIDES ANTIPSYCHOTICS LEAD TO TARDIVE DYSKINESIA?
Yes, but not usually. The only non-antipsychotic medication that regularly causes TD is levodopa.
Levodopa is a medication that increases the stimulation of dopamine receptors. Amphetamines, which are
types of stimulant medications that increase the stimulation of dopamine receptors, have also been linked
to TD. Benztropine (Cogentin), a medication that also increases the stimulation of dopamine receptors,
has been linked to TD.
Another medication known to lead to TD (especially in the elderly) is Metoclopramide (Reglan). This
medication is given to decrease nausea and vomiting and to increase peristalsis. Peristalsis is a series of
wavelike, coordinated contractions and relaxations of a tube-like structure (such as the intestine) in the
body that forces the contents of the tubes onwards. The intestine is a tube shaped structure that is part of
the digestive tract.
Antihistamines have also been reported to cause TD. Histamine is a natural substance in the body that is
released during allergic reactions and leads to many allergic symptoms. Substances that block the effects
of histamine are known as antihistamines and are used to treat allergies. Some antidepressant
medications (such as Prozac) have also been reported to cause TD.
HOW MANY PEOPLE DEVELOP TARDIVE DYSKINESIA?
There are at least 300,000 people in the U.S. with TD. TD occurs in approximately 14 to 30% of patients
that are given antipsychotics over a long period of time (at least three months). Elderly patients taking
antipsychotics between 3 and 12 months have been shown to have a 29% chance of developing TD. If
taking antipsychotics for as long as five years, about 20 to 40% of patients will develop TD. One study
found that elderly patients taking antipsychotics for more than 10 years have a 41% chance of developing
TD. Other research has shown that elderly patients (over age 55) who took antipsychotic medications for
1, 2, and 3 years had a 25%, 34%, and 53% chance of developing TD, respectively. The frequency of
people developing TD is similar in other countries besides the U.S.
ARE THERE RISK FACTORS FOR TARDIVE DYSKINESIA?
Yes. The main risk factors for TD are age and length of antipsychotic use. That is, elderly patients (over
age 55) have a greater risk of developing TD than younger patients. Also, patients using antipsychotics
for long periods of time have a greater chance of developing TD than patients using antipsychotics for
short periods of time. From this, it makes sense that older patients taking antipsychotics for long periods
of time are at high risk for developing TD.
It has been found that patients younger than 60 are three times more likely to have TD go away without
treatment. Older patients are more likely to develop abnormal involuntary movements in the mouth and
face whereas younger patients are more likely to develop abnormal involuntary movements in the arms,
legs, and trunk.
TD generally affects older people who are treated for long periods (about one year) with phenothiazines,
which are types of drugs used to treat psychosis, allergies, and vomiting. Names of some pheonthiazines
include: Chlorpromazine (Thorazine), Fluphenazine (Permitil, Prolixin), Mesoridazine (Serentil),
Perphenazine (Trilofan), Thioridazine (Mellaril), Trifluoperazine (Stelazine).
Patients that use depot neuroleptics may have a greater chance of developing TD than patients who take
antipsychotics by mouth. Depot neuroleptics are an injected form of an antipsychotic drug that stays in the
muscle and slowly releases itself overtime. Patients that have had sudden adverse effects to
antipsychotics or other drugs that block dopamine receptors are also more likely to develop TD. Being on
antipsychotics that are stronger at blocking dopamine-2 receptors appears to put one at greater risk for
TD than being on drugs that are weaker at blocking dopamine-2 receptors.
TD is mostly seen in patients with schizophrenia, schizoaffective disorder, or bipolar disorder, who are
treated with antipsychotic medications. Schizophrenia is a type of mental disorder in which one loses
contact with reality. Schizoaffective disorder is a combination of schizophrenia symptoms and a mood
disorder (such as depression or mania). Mania is the extreme opposite of depression, in which the person
experiences signs symptoms such as extreme excitement, hyperactivity, overtalkativeness, agitation,
and/or dangerous behavior. Bipolar disorder is a mental condition characterized by episodes of mania,
depression, or mixed moods.
People with schizophrenia that are exposed to poisonous substances are at risk to develop TD. It has
been suggested (but not proven) that schizophrenic patients who have family members with mood
disorders (such as depression) and the presence of depressive symptoms are at increased risk for TD.
Patients with a history of abnormal involuntary movements (that are not at the level of TD) in reaction to
antipsychotics have an increased risk of developing TD in the future if given antipsychotics again.
Patients who have had family members that developed TD after taking antipsychotics for a long period of
time are at increased risk to develop TD. Patients that smoke are also at increased risk to develop TD.
Patients who have suffered from a long-term illness also have an increased risk of developing TD.
Examples are patients with mental retardation and psychosis, alcoholism, and epilepsy with psychosis.
Epilepsy is a brain condition that is characterized by changes in sensation, abnormal behaviors, loss of
consciousness, convulsive seizures, or all of these. Convulsive seizures are sudden abnormal, severe
involuntary muscle movements, with a racing heart and other symptoms.
TD is more likely to occur in African-Americans. People with other movement disorders are more likely to
develop TD, as are patients with diabetes mellitus. Diabetes mellitus (often abbreviated as DM) is a
complex, long-term disorder in which the body is not able to effectively use a natural chemical called
insulin. Insulin's main job is to quickly absorb glucose (a type of sugar) from the blood into cells for their
energy needs and into the fat and liver (a large organ that performs many chemical tasks) cells for
storage.
CAN CHILDREN DEVELOP TARDIVE DYSKINESIA?
Yes. Children can develop TD, but it is much more common for elderly people to develop TD.
WHICH ANTIPSYCHOTIC MEDICATIONS ARE MOST LIKELY TO CAUSE TARDIVE DYSKINESIA?
All antipsychotic medications put one at risk for developing TD if taken for an extended period of time.
However, tardive dyskinesia is more common with older antipsychotics (known as typical antipsychotics)
as opposed to the newer antipsychotics (known as atypical antipsychotics). Unlike typical antipsychotics,
atypical psychotics are better at blocking serotonin receptors and do not block as many dopamine-2
receptors in the nigrostriatal pathway. As was discussed in the section on causes of TD, blocking
dopamine receptors in this pathway can lead to TD.
Atypical antipsychotics are better at blocking dopamine receptors in a different pathway that is more likely
to relieve the signs and symptom of psychosis. This pathway is known as the mesolimbic pathway. The
mesolimbic pathway is a pathway in the brain that connects the midbrain ventral tegmental area (an area
in the lower part of the brain) to the nucleus accumbens. The nucleus accumbens is a part of the brain
thought to be responsible for pleasurable feelings (particularly during drug abuse), delusions (false beliefs,
despite clear evidence to the contrary of those beliefs), and hallucinations (sensations that are not really
present).
The above information explains why atypical psychotics are less likely to lead to TD than typical
antipsychotics. That is, since blocking dopamine-2 receptors in the nigrostriatal pathway is what leads to
TD, and since atypical antipsychotics are less likely to do this, this means that atypical antipsychotics are
less likely to lead to TD. Some of the antipsychotic medications that are more likely to cause TD include
Haldoperidol (Haldol), Fluphenazine (Prolixin), and Chlorpromazine (Thorazine). Newer antipsychotics like
Risperidal have also been known to cause TD, however, in less frequency.
HOW SERIOUS IS TARDIVE DYSKINESIA?
TD is potentially a very serious condition. It can lead to difficulty breathing due to abnormal jerking
movements in the belly area and the diaphragm. The diaphragm is a muscular-fibrous area that separates
the chest and abdomen that assists in breathing. The motor problems caused by TD can make it
impossible to eat, difficult to stand, and difficult to walk. TD can also lead to ulcers in the mouth. An ulcer
is an open sore on the skin or on a mucous membrane. A mucous membrane is one of four major types of
thin sheets of tissue that line or cover various parts of the body, such as the mouth and passages for
breathing.
HOW IS TARDIVE DYSKINESIA TREATED AND MANAGED?
At present, there is no accepted treatment for TD. Treatment is decided upon on a case-by-case basis,
but the main goal is typically to decrease dopamine activity. You may be wondering why this is so, since
antipsychotics block dopamine receptors in the first place. But it must be remembered that one of the
explanations for TD is that an oversensitivity to dopamine exists in those dopamine receptors that are not
blocked or in the extra receptors that were produced. Thus, decreasing dopamine activity would have the
effect of decreasing the oversensitivity to dopamine caused by antipsychotics.
The problem is that decreasing the sensitivity to dopamine does not always reduce the severity of TD.
This has also led others to criticize the hypothesis that oversensitive dopamine receptors lead to TD.
Sometimes the first step in treating TD is to stop or decrease the administration of the drug (in 10%
increments) that is causing the problem. This may not be a reasonable choice, however, if the patient is
taking the drug because of a severe condition. Most doctors choose to slowly decrease the drug while
observing the patient as opposed to stopping it altogether.
Stopping the antipsychotic all of a sudden can increase the severity of the psychosis, increase the risk of
suicidal and/or homicidal behavior, and cause the patient to be hospitalized. The risk of having a
permanent movement disorder needs to weighed against the risk of having an uncontrolled psychotic
disorder. Another factor to consider is that TD may remain or get worse long after the antipsychotic drugs
have been discontinued.
Many doctors choose to administer an atypical antipsychotic, usually Clozapine (Clozaril), to patients with
TD that need to be on an antipsychotic. Why not just give all patients Clozaril in the first place? The
reason is because patients on Clozaril are at risk for developing a deadly condition known as
agranulocytosis, which is a severe reduction in the numbers of white blood cells. White blood cells help
defend the body against infections.
Some doctors treat TD by increasing the amount of dopamine in the brain by prescribing medications,
such as levodopa, that increase the stimulation of dopamine receptors. It was mentioned in a previous
section that levodopa can actually cause TD, which is true. Interestingly, levodopa has the ability to both
cause and treat TD, depending on the particular patient.
Alpha-methyl-p-tyrosine (AMPT) is a drug that decreases the production of dopamine in the brain and has
been used to decrease abnormal involuntary movements in TD. Benztropine (Cogentin), a medication that
also increases the stimulation of dopamine receptors, has also been used to treat TD. However, many
doctors advise againt using this drug to treat TD because it can actually make the condition worse.
It is not entirely clear why some drugs that both decrease and increase dopamine receptor stimulation can
treat TD. Conflicting research findings may be due to different research methodologies, different criteria to
define TD, different research designs, different drug doses, and other factors.
Many doctors use vitamin E to treat the symptoms of TD. Although the usefulness of treating TD with
vitamin E is doubtful, its safety makes it an easy choice for doctors. Vitamin E is thought to treat TD by
destroying harmful chemicals in the body known as free radicals. The free radicals are thought by some to
cause damage in the brain that leads to TD.
Sometimes, replacing the drug that is causing TD with a different type of drug may improve the condition.
Adrenergic antagonists, which are drugs that stimulate norepinehrine, have been used to treat TD.
Norepinephrine is a type of chemical messenger that helps to increase blood pressure.
Botox (botulinism toxin) has also been used to treat TD because it prevents certain muscle movements.
Ondansetron (Zofran), which is a medication that blocks a chemical in the brain known as 5-
hydroxytryptamine-3, has also been used to treat TD. Another medication used to treat TD is the mood
stabilizing drug, Lithium. However, the effectiveness of using Lithium to treat TD is questionable.
Some doctors treat TD by administering medications (such as choline chloride and lecithin) that increase
the amount of acetylcholine (another type of chemical messenger important for muscle movements). The
goal of this type of treatment is to restore the balance between dopamine and acetylcholine in the brain.
Drugs that increase the chemical messenger GABA (gamma-aminobutyric acid), such as Clonazepam
(Klonopin), has also been used to treat TD. GABA works by inhibiting (decreasing) the effect of dopamine.
Drugs that increase GABA are typically used to treat depression because of their calming effects. Another
type of antianxiety drug known as Buspirone (Buspar) has been used to treat TD. Buspar both blocks and
stimulates dopamine receptors.
Some doctors advocate increasing the dosage of antipsychotic medications in patients with TD. The
purpose of this is to block the oversensitive dopamine receptors that have been produced by the
antipsychotic medications. Some research has shown that this technique works with some patients.
However, it may not work well over the long-term. Some have suggested only using this technique with
Clozaril. Deciding whether or not this technique will be helpful depends on the specific case.
As was mentioned earlier, the abnormal movements of TD should decrease when a particular body part is
activated. For example, placing the patient's fingers on his/her lips can stop abnormal movements of the
lips. However, if the person voluntarily tries to move an area affected by abnormal movements, this can
make the TD worse.
Emotional stress and mentally trying to stop the abnormal movements can also make TD
worse. Thus, reducing stressors are important in managing TD and it is important for
patients to try to avoid stopping the abnormal movements, even though the movements may
be frustrating to them. Patients with TD will often need long periods of rest because the
involuntary motor movements often cause tiredness. TD movements decrease when the
person is relaxed and disappear when the person sleeps.
CAN TARDIVE DYSKINESIA BE REVERSED?
Although many descriptions of TD state that the condition is irreversible, this is not always
true. In general, the earlier TD is recognized and the earlier the antipsychotics are
discontinued (if appropriate), the greater the chance that TD will go away. Some studies
found that TD goes away in weeks after antipsychotics are discontinued in young patients.
For example, one study showed that 33% of patients who were treated with the
antipsychotic, Clozaril, no longer had TD after 100 weeks. Research has also suggested
that Clozaril is not masking the TD because the TD was still gone when the patients were
taken off of Clozaril. The same is true for another atypical antipsychotic, Olanzapine
(Zyprexa), used to treat TD.
If a schizophrenic patient with TD is switched from a typical antipsychotic to an atypical
antipsychotic, some of the cases of TD will go away. Click here for a description of typical
and atypical antipsychotics. If the antipsychotic medication is totally stopped, this helps TD
go away in about 60% of cases. It should be noted that there are also some cases of TD
that go away spontaneously.
So why is it that so many people describe TD as always irreversible? The answer seems to
lie in history. In the first article describing a case of TD, the authors described the condition
as irreversible. This is interesting considering that only 65% patients in that study were
found to still have the condition upon follow-up between 4 and 22 months. Nevertheless, it
seems that people continue to carry on the myth that TD is irreversible, as the first authors
on the topic incorrectly stated. The reference for this article is: Uhrbrand L, Faurbye A
(1960). Reversible and irreversible dyskinesia after treatment with perphenazine,
chlorpromazine, reserpine, ECT therapy. Psychopharmacologia 1:408-18.
CAN TARDIVE DYSKINESIA BE PREVENTED?
To some degree, TD can be prevented. This can be done if the doctor prescribes the lowest effective
amount of antipsychotic medications for the shortest period of time. If the antipsychotic is not working,
there is no reason to be on it because it may increase the risk of developing TD. Prescribing other
medications to treat sleep disorders and anxiety besides antipsychotics can decrease TD.
As was described in a previous section, using atypical antipsychotics as opposed to typical
antipsychotics seems to decrease the chances of developing TD. Some research has suggested that TD
can be avoided by giving the patient vitamin E, but it is not known if this really works.
Patients and family members should keep in touch with the doctor who prescribed the medications so that
their effects are closely monitored. Patients and family members should be clear as to how long the
antipsychotic medication will be prescribed. Being alert to the signs of TD can also be helpful in identifying
the problem early.
WHEN WAS THE TERM, "TARDIVE DYSKINESIA," FIRST USED?
The term, "tardive dyskinesia," was first used in 1964. However, the first case report of TD (although it
was not called this back then) was by Uhrbrand and Faurbye. The reference for this article is: Uhrbrand L,
Faurbye A (1960). Reversible and irreversible dyskinesia after treatment with perphenazine,
chlorpromazine, reserpine, ECT therapy. Psychopharmacologia 1:408-18.
WHAT ELSE IS TARDIVE DYSKINESIA KNOWN AS?
TD is also known as lingual-facial-buccal dyskinesia.
WHAT IS THE ORIGIN OF THE TERM, TARDIVE DYSKINESIA?
Tardive dyskinesia comes from the Greek word "tardus" meaning "late," the Greek word "dys" meaning
"difficult," and the Greek word "kinesis" meaning "movement." Put the words together and you have "late
(and) difficult movement(s)."