MedFriendly®


Human Papillomavirus
Human papillomavirus (commonly abbreviated HPV) is a
common disease that often causes warts on the reproductive
organs and skin (often on the hands and soles of feet),
papillomas, or damage to the mucous membranes of the
mouth, genitals, and anus (the area that poop comes out of).
A wart is a type of visible growth on the body caused by a
virus. A mucous membrane is one of four major types of thin
sheets of tissue that line or cover various parts of the body.
FEATURED BOOKS: Human Papillomaviruses
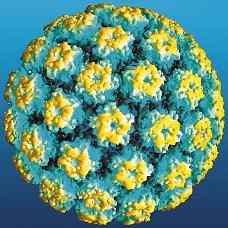
HPV magnified.
or is round in shape. Benign means that the abnormality stays in a localized area of the
body and does not invade surrounding tissues. Epithelium is a group of cells that occur in
one or more layers, which cover the entire surface of the body and line most of the
hollow structures in it. A papilloma is not a form of cancer. Cancer is an abnormal growth
of new tissue characterized by uncontrolled growth of abnormally structured cells that
have a more primitive form.
WHAT ARE THE DIFFERENT TYPES OF HPV AND HOW ARE THEY CLASSIFIED?
There are more than 100 different types of HPV, most of which are harmless. Each type
of HPV is labeled in number format. For example, the first type of HPV is known as HPV-
1, the second type is known as HPV-2, and so on. Some types of HPV are only found on
certain parts of the skin or mucous membranes.
"Where Medical Information is Easy to Understand"™
The different types of HPV are divided into three main categories.
The first category is called anogenital and/or mucosal. These types
of HPV cause warts on the anus, genitals, and/or mucous
membranes. A mucous membrane is one of four major types of thin
sheets of tissue that line or cover various parts of the body. About
23 types of HPV affect the genitals in males and females.
Anogenital and/or mucosal types of HPV are most common in
college-aged women or men. Women are more likely to have the
anogenital/mucosal form of HPV than men. For every male that has
anogenital/mucosal HPV, 1.5 females have this type of HPV.
Anogenital warts are most common in moist areas but can occur on
dry areas as well.
The second category of HPV is known as nongenital cutaneous because they cause warts on the skin,
but not on the genitals. The word "cutaneous" refers to skin. Common warts are caused by HPV types 1,
2, 4, 26, 27, 29, 41, 57, and 65. These warts can occur anywhere on the body, but usually occur on the
hands and fingers. These warts are usually skin-colored, rough, and bumpy masses that grow outwards
and have slight scaling. These warts can be spread to other parts of the body when the person touches
him/herself with a wart. For example, if a wart on a person's finger touches the finger next to it, that
finger may develop a wart.
Flat warts are caused by HPV types 3, 10, 27, 28, 38, 41, and 49. These warts usually occur in small
groups on the face and hands. They are usually less than five millimeters wide. A millimeter is a very
small unit of length equal to .0394 inches. These warts usually go away by themselves after several
years. Several weeks before these types of warts disappear, itching and redness usually occurs in the
affected area.
Warts on the bottom of the foot are caused by HPV types 1, 2, 4, and 63. These warts can become
black and painful before going away by themselves. These warts may contain small seed-like
substances, which are actually capillaries with clots (masses of blood) in them.
Capillaries act as an exchange system that connects the smallest veins (known as venules) with the
smallest arteries (known as arterioles). Veins are blood vessels that carry blood to the heart. Arteries
are blood vessels that carry blood away from the heart to the rest of the body. Venules and arterioles
are other types of small blood vessels.
Bucther's warts are caused by HPV types 1, 2, 3, 4, 7, 10, and 28. Butcher's warts are warts that occur
in people who handle meat, poultry, and fish. These warts are often large and have the appearance of
cauliflower. Nongenital skin warts are most common in teenagers and adults who handle meat, poultry,
and fish. About 10% of children and young adults develop butcher's warts each year. Nongenital skin
warts rarely occur before age 5.
Mosaic warts are caused by HPV types 2, 27, and 57. Mosaic warts are numerous warts on the bottom
of the foot that are located closely together and form a mosaic appearance. Mosaic is a descriptive
term for something that appears to be made up of many tiny pieces or bits that are close together.
The third category of HPV is known as epidermodysplasia verruciformis (EV). Types of HPV in this
category cause EV, which is a rare disease characterized by numerous flat warts on the hands and feet.
EV can be non-cancerous or can become cancerous. The non-cancerous form is caused by HPV types
2, 3, 10, 12, 15, 19, 36, 46, 47, and 50. The cancerous types are caused by HPV types 5, 8, 9, 10, 14,
17, 20, 21, 22, 23, 24, 25, 37, and 38.
People with decreased body defenses are more likely to develop an EV type of HPV infection,
especially if they have skin cancer. EV usually begins at age 6 and beginning between age 40 and 50.
Thus, the condition develops slowly. The warts that develop in EV can become cancerous. Development
into cancer is most likely to happen if the patient is exposed to radiation (a form of energy in the form of
waves or streams of particles), such as from the sun or from x-rays. Noncancerous forms of EV usually
occur on the forehead or other areas of the body exposed to the sun.
The mucosal category of HPV is further divided into latent types (no signs present), subclinical (so mild
that it produces no visible signs), or clinical (noticeable signs present). Subclinical types can only be
identified with a microscope. Clinical types produce very noticeable signs.
WHAT CONDITIONS ARE HPV ASSOCIATED WITH?
The conditions associated with HPV depend on the type of HPV the person has. Different combinations
of factors lead to the many different ways that HPV can present itself. Some forms of HPV are
associated with cancer. Cancer of the cervix (also known as cervical cancer) is the least common, but
most serious result of HPV infection.
The cervix is a small, cylinder-shaped organ that forms the lower part and neck of the uterus. The uterus
is a hollow organ in a female's body where the egg is implanted and the baby develops. HPV is the main
cause of cervical cancer and other diseases of the cervix. In fact, almost all cases of cervical cancer
are caused by HPV. HPV can also cause cancer in other areas of the genitals.
Cancer of the cervix has been associated with HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59,
68, and 69. These types of HPV are known as "high-risk" types because they lead to a high risk of
developing cervical cancer in both males and females. In fact, high-risk types of HPV are found in
between 95% to 99.7% of cervical cancer cases throughout the world. However, it is important to
realize that having a high-risk type of HPV does not give you a 95% chance of developing cervical
cancer. It just means that having this type of HPV puts you at an increased risk to develop cervical
cancer. HPV is a known carcinogen (cancer causing subtance) and is a type of oncovirus (cancer
causing virus).
High-risk types of HPV that are associated with cancer can lead to flat abnormal growths of tissue that
are different from the characteristic appearance of warts. In fact, these flat abnormal growths are often
not visible to the naked eye. It should be noted that when taking into account all of the different types of
HPV, most cases do not lead to abnormal growths or cervical cancer.
Cancer of the cervix usually takes years to develop. Up to 66% of preventable cervical cancer cases
occur in women who have never had a Pap smear or who have not had one in 5 years or more. A Pap
smear is a type of test used to detect abnormal changes in cells. This is done by scraping away loose
cells from the cervix, spreading (smearing) it on a glass slide, and examining it under a microscope.
Women who develop HPV are at greater risk for cervical dysplasia, which is a pre-cancerous condition
that can develop into cervical cancer. Cervical dysplasia is also known as cervical intraepithelial
neoplasia (CIN). Cervical dysplasia can be treated but is monitored by yearly Pap smears. However, it
is possible for aggressive types of cancers to develop between Pap smears.
A type of cervical dysplasia associated with HPV is a squamous intraepithelial lesion. A squamous
intraepithelial lesion (commonly abbreviated SIL) is a general term for the abnormal growth of squamous
cells on the surface of the cervix. Squamous cells are flat, scale-like types of epithelial cells. Epithelial
cells are cells that help absorb, move, and distribute some of the fluids and nutrients in the body.
Squamous intraepithelial lesions are classified as low grade or high grade. A low grade squamous
intraepithelial lesion (commonly abbreviated LGSIL) is one in which the cells are not very abnormal and
not much of the cervix is affected. A high grade squamous intraepithelial lesion (commonly abbreviated
HGSIL) is one in which the cells are very abnormal and much of the cervix is affected. LGSIL's are
caused by HPV types 6, 11, and 43.
HPV types 16 and 18 are responsible for most HGSIL's, but types 56 and 58 can also cause it. HGSIL's
can develop into carcinomas, especially those in the anogenital and/or mucosal category (see above). A
carcinoma is any malignant cancer that arises from cells in the covering surface layer or membrane
(outer covering) that lines an organ of the body. When describing cancer, malignant means that the
newly formed tissues are made of abnormally structured and primitive-looking cells that grow
uncontrollably, spread throughout the body, and invade surrounding tissues.
Many types of HPV are associated with warts on the outside of the genitals, on the skin around the
anus, on the inside and outside of the vagina, but not on the cervix. Because these types of warts are
not usually associated with cancer of the cervix, the types of HPV that cause them are known as "low-
risk" types.
Examples of low-risk types of HPV are types 6 and 11. These two types of HPV are commonly
associated with genital warts. In women with cervical cancer, low risk types of HPV are rarely ever
found. Low risk types of HPV are more likely to cause genital warts or other types of infections.
It is possible for warts to occur on the cervix or the vagina. The vagina is an opening in the female's
body that is part of the reproductive system. Warts on different body parts are due to different types of
HPV. It can take several months or several years to develop warts after someone contracts HPV.
Genital warts do not lead to cervical cancer. However, they grow outwards and can often be unsightly
and uncomfortable due to their cauliflower-like appearance. Genital warts can be smooth and bumpy or
have a thickened horny layer. The warts on the outside of the genitals or anus that are caused by HPV
are known as venereal warts or condylomata acuminata. These warts are caused by HPV types 6, 11,
30, 42, 43, 44, 45, 51, 52, and 54.
There are about 30 types of HPV that are linked to infections of the genitals. Different types of HPV
cause warts on the genitals than those that cause warts on the hands and feet. Rarely, warts caused by
HPV can occur in the mouth or throat of a person who has had sex with an infected individual.
HPV types 16 and 18 can cause carcinoma of the larynx. The larynx is an organ located at the upper
part of the windpipe that produces voice. HPV types 6, 11, and 30 can cause papillomas of the larynx.
Carcinomas can occur in squamous cells of the fingernails and lungs. The squamous cell carcinomas of
the fingernails can be caused by HPV type 16. The squamous cell carcinomas of the lung can be caused
by HPV types 6, 11, 16, and 18.
HPV types 6 and 11 can cause numerous papillomas (see above) to develop in the respiratory system
(the system of the body that helps people breathe). HPV type 57 can cause papillomas to develop in the
maxillary sinus. Sinuses are openings in the bones that often contain fluid. The maxillary sinus is a sinus
in the upper jaw. HPV types 16 and 18 can cause carcinomas to occur in squamous cells of sinuses and
the esophagus. The esophagus is a tube-shaped structure that takes food down into the stomach after it
is swallowed.
HPV types 6 and 11 can cause papillomas and warts to develop in the front of the nostrils, mouth,
larynx, and conjunctiva. The conjunctiva is a clear layer that covers and protects the inside of the
eyelids and the front part of the sclera (the white part of the eyes). HPV type 16 can cause carcinomas
in the conjunctiva. HPV types 16 and 18 can cause carcinomas and leukoplakia to develop in the mouth.
Leukoplakia is a precancerous, slowly developing change in mucous membranes that is characterized
by thick, white, firmly attached patches that are slightly raised and within a well-defined area.
HPV types 13 and 32 can also cause Heck disease. Heck disease is multiple, soft, abnormal, knob-
shaped tissues that form on the lips, mucous membranes of the cheek, tongue, and other areas of the
mouth. Bowen disease can be caused by HPV types 16, 18, 31, and 34. Bowen disease is a type of
carcinoma in the skin that is characterized by the development of slowly enlarging pink or brown papules
(small, enlarged abnormal areas of tissue) or worn away plaques covered with a thickened horny layer.
Plaques are flat, and often raised abnormal patchy areas on the skin. Papules can occur on the genitals
of males and females. This is known as Bowen's papulosis and can be caused by HPV types 16, 18, 34,
39, 42, and 45.
HPV is also associated with penis cancer, anus cancer, cancer of the vagina, and cancer of the vulva.
The vulva is the outer, visible part of the female genitals. Penis cancer, which is rare, is caused by HPV
types 16 and 18. Anus cancer and cancer of the vagina are caused by HPV types 16, 31, 32, and 33.
About 88% of the cases of anus cancer throughout the world are due to HPV. Cancer of the vulva is
caused by HPV types 6, 11, 16, and 18.
HPV can cause some cancers of the oropharynx. The oropharynx is the middle part of the throat that
includes the bottom of the tongue, the tonsils, and the soft palate. The tonsils are a pair of oval masses
at the back of the throat. The soft palate is the back part of the roof of the mouth.
HOW DOES HPV CAUSE CANCER?
Some types of HPV may cause cancer by producing proteins (known as E5, E6, and E7) that interfere
with other proteins that normally prevent excessive cell growth. Excessive cell growth is a defining
characteristic of cancer. As an example, HPV type 6 produces a protein that interferes with a protein
known as p53, which prevents excessive cell growth.
HPV does not cause cancer by itself. Factors such as smoking, unprotected sun exposure, having many
children, pregnancy, the use of birth control pills, and a deficient amount of folate can interact with the
status of the body's defense system to determine how the signs of HPV infection present and whether
cancer develops. Folate is a salt of folic acid (a type of vitamin).
A decreased amount of folate seems to help the DNA of HPV move into a fragile chromosome site. This,
in turn, provides a basis for malignant skin abnormalities to develop. DNA is a chain of many connected
genes. Genes are tiny structures that contain coded instructions for how proteins should be constructed
and how certain bodily characteristics should develop. Genes are contained in structures called
chromosomes.
HOW DO PEOPLE GET HPV?
About 33% of HPV types can be passed on from person to person through sexual contact. Sexual
activity is most commonly associated with higher risk for anogenital and/or mucosal types of HPV.
During sexual intercourse or after minor scraping of the skin, the epithelium can become disturbed,
allowing HPV to come through and cause an infection. Epithelium is a group of cells that occur in one or
more layers, which cover the entire surface of the body and line most of the hollow structures in it.
In the United States, HPV is the most common sexually transmitted virus disease in both men and
women. It is one of the common sexually transmitted diseases in the world. About 30 types of HPV can
be spread through sexual contact.
Some studies have estimated that most sexually active people are exposed to at least one or more
types of HPV. All forms of sexual intercourse, including anal and oral sex are all capable of spreading
HPV. Even foreplay can lead to the spreading of HPV and cause warts to develop on the hands or in the
mouth. The virus passes through skin contact with an infected person, such as touching an infected
wart.
Having sex at an early age (especially age 16 or younger) or having many sexual partners leads to an
increased chance of getting HPV. One does not need to have many sexual partners to come in touch
with the virus since it is so common. Having sex with a partner that has or has had many sexual
partners increases the chance of getting HPV. Someone is most likely to pass on HPV after he/she first
gets the virus.
It is more common for HPV to be spread through sexual intercourse in women who have visible warts. In
fact, about 66% of people who have sexual contact with a person with genital warts will develop HPV.
This usually happens within three months of contact with the genital warts.
It is also true that about half of people that have HPV never develop genital warts. HPV can be passed
on from people who do not have warts or who have had warts in the past. This indicates that the virus is
passed on through body fluids, such as fluids in the cervix or semen. If a person or his/her partner has a
history of genital warts, sexually transmitted diseases, cervical cancer, penis cancer, or abnormal Pap
smears, it increases the chance of getting HPV.
Just one episode of unprotected sexual activity with a person that has HPV carries a 60% risk of being
infected with this virus. Women with another type of sexually transmitted virus known as HIV (human
immunodeficiency virus) who also have HPV have a 40% greater risk of developing severe
abnormalities in the cells of the cervix compared to women with HPV that do not have HIV. People with
HIV and lowered body defenses are more likely to develop HPV. People with lowered body defenses are
especially likely to be infected with HPV if they have skin cancer.
Sexual contact is not the only way to spread HPV. For example, if someone with HPV-related warts on
the bottom of the feet walks barefoot, he/she can spread this virus. This is because HPV can survive for
months in cold temperatures without a host (organism to live in or on). When another person walks on
the area of the floor that the barefoot person walked, he/she can get infected with the virus on the floor.
CAN GENITAL WARTS SPREAD?
Yes, genital warts can be spread from person to person because they are very contagious. In fact,
about 66% of people who have sexual contact with people that have genital warts will go on to develop
genital warts within three months. Genital warts usually occur in groups or clusters and can take on
many different types of appearances. Even though the warts (or a wart) can initially be very tiny and not
visible, they can spread into large masses on the genitals or anus. The warts can eventually take on a
fleshy, raised appearance that looks like cauliflower. Warts can also be flat.
HOW MANY PEOPLE HAVE HPV?
As was mentioned earlier, HPV is the most common sexually transmitted disease in the United States.
According to the American Social Health Association, there are about 5.5. million new sexually
transmitted cases of HPV a year. It is estimated that at least 20 million Americans are already infected
with HPV. There may be as many as 40 million Americans with HPV. For women ages 20 to 30,
approximately 15% carry HPV. For women over age 40, approximately 6% carry HPV.
The number of people with HPV over the past few years has increased significantly due to increased
awareness of the many types of HPV and because of better techniques to diagnose it. The percentage
of women with an HPV infection in a given year is estimated to be between 22 and 35%. The
percentage of men with an HPV infection in a given year is estimated to be between 2 and 35%,
depending on the sexual practices of the population being studied.
ARE CERTAIN RACES MORE LIKELY TO GET HPV AND WARTS THAN OTHERS?
HPV is more common in African-Americans, Native-Americans, and Hispanics. However, nongenital skin
warts are more common in whites than African-Americans.
HOW LONG DOES IT TAKE TO SHOW SIGNS OF HPV INFECTION?
From the time HPV is transmitted, it can take weeks to years for signs to develop. Women infected as
teenagers may not show signs of infection until age 30 or 40, or may not show signs at all. About half of
people with HPV do not present with any signs or symptoms. This is because the immune system of
many people is capable of fighting off HPV. Thus, it is possible to have HPV and not be aware of it. This
can lead for people to spread HPV unknowingly.
DOES HPV AFFECT THE ABILITY TO GIVE BIRTH?
No. HPV should not affect the ability to give birth. However, since pregnancy normally decreases a
woman's immune system, HPV infections can flare-up in pregnant patients. It is possible for HPV to be
transmitted from the mother to the baby during pregnancy, but this is rare. For this reason, however,
pregnant mothers should inform the doctor if they have HPV or have had it in the past.
Genital warts can cause some problems in pregnancy. For example, due to changes in hormone levels
during pregnancy, genital warts can get larger, making it difficult to pee. Hormones are natural chemicals
produced by the body and released into the blood that have a specific effect on tissues in the body.
Warts in the vagina can make it less stretchy, causing a blockage during delivery. If the warts are not
removed, a cesarian section (c-section) may be needed to deliver the baby. A c-section is when the
belly and uterus are cut open so that the baby can be delivered through the belly.
In rare cases, infants born to women with genital warts can develop genital warts in their throats, which
are known as laryngeal papillomatosis. In these cases, HPV appears to be passed on to the child when
he/she passes out of the birth canal of the infected mother. The warts in the throat usually occur at age
3 and are associated with hoarseness. The warts can threaten the infant's life because they can block
the breathing passages in the throat. Laser surgery can prevent such a blockage from occurring. Infants
can also develop warts on the genitals and anus.
Immediately after birth, some infants may have substances in their nasopharynx from the mother that
contain HPV. These infants are usually not considered infected because the virus usually clears from
the infant in a few months. The nasopharynx is the part of the pharynx that lies above the soft palate.
The pharynx is a passage that connects the back of the nose and mouth to the esophagus. The soft
palate is the back part of the roof of the mouth.
CAN MALES GET HPV?
Males can get HPV, but it often is not associated with any health risks. Genital warts can occur in men,
but it is less common than women. When HPV causes warts in men, the warts usually occur around the
anus, scrotum, or on and under the foreskin of the penis. The scrotum is the pouch of skin that contains
the testicles. The foreskin is the loose fold of skin that covers the end of the penis. It is possible for
HPV to cause cancer in men.
HOW IS HPV DIAGNOSED?
No single test has been shown to be totally reliable in diagnosing HPV. Currently, the diagnosis of HPV
is based on a Pap smear (see earlier section), a colposcopy, and a biopsy. HPV is one of the most
common causes of abnormal Pap smears. In fact, about 25% of all abnormal Pap smears are due to
HPV. A colposcopy is a visual examination of the vagina and cervix with a lighted magnifying instrument,
known as a colposcope. A colposcopy can also help identify flat genital warts on the cervix that are not
yet visible to the naked eye.
A biopsy is the process of removing living tissue (such as warts) or cells from organs or other body
parts of patients for examination under a microscope or in a culture to help make a diagnosis, follow the
course of a disease, or estimate a prognosis. A culture is an artificial way to grow cells or tissues in the
laboratory. It should be noted, however, that HPV cannot be cultured.
A biopsy of a wart is often done if it has not gone away with treatment, if the person with the wart has
lowered body defenses, or if the warts get better with treatment. Biopsies are useful when the diagnosis
of HPV is uncertain, especially if the warts are abnormally colored, hardened, or form into an ulcer (open
sore).
A biopsy can help detect the DNA of HPV in the tissue sample. The test that does this is known as
Hybrid Capture System HPV DNA Assay (also known as Digene's HPV test). It is the most advanced
technique currently available to detect HPV and can detect this virus even before abnormal cell changes
become visible. This test can only be used on women.
DNA is a chain of many connected genes. Genes are tiny structures that contain coded instructions for
how proteins should be constructed and how certain bodily characteristics should develop. The reason
why Pap smears are not completely reliable in detecting HPV is because they are not designed to
specifically look for the DNA of this virus.
In low-risk-HPV types, the genetic code of HPV exists as a circular type of DNA that is separate from
the nucleus (central structure) of the host cell. The host cell is the name for the cell that HPV lives in. In
high-risk HPV types, the genetic code of HPV is combined with the DNA of the host cell. When the
genetic code of HPV combines with the genetic code of the host cell, cancer can result.
Since HPV only multiplies in the nucleus of affected cells. The nuclei of affected cells have a very
abnormal appearance under the microscope. An example of such an abnormality is koilocytosis.
Koilocytosis refers to the presence of squamous cells that often have two nuclei and small holes near
the nuclei. The presence of koiliocytosis is characteristic of the human papillomavirus (HPV) infection.
Another lab finding consistent with HPV is dyskeratosis. Dyskeratosis is the premature keratinization of
individual epithelial cells that have not reached the surface layer where keratinization normally occurs.
Keratinization is the formation of keratin. Keratin is a type of protein that is the main component of the
outermost layer of the skin, nails, and hair. Epithelial cells are cells that help absorb, move, and
distribute some of the fluids and nutrients in the body.
Yet another lab finding consistent with HPV is acanthosis. Acanthosis is an increase in the thickness of
the stratum spinosum of the epidermis. The epidermis is the top layer of the skin that does not contain
blood vessels. The stratum spinosum is a layer that is located approximately in the middle of the
epidermis.
The type of cells that comes back as abnormal on a Pap smear result are often flat scale-like cells
known as squamous cells. The doctor is often not sure if the abnormal results are serious or not. The
term used to describe this type of abnormal result is ASCUS (abnormal squamous cells of uncertain
significance).
Diagnosing HPV in women with ASCUS is useful to do because it helps identify which individuals need
to be followed-up more intensively for changes in cells that may develop into cancer of the cervix in the
future.
WHAT ARE SOME PROBLEMS WITH HPV DIAGNOSIS?
The main problem with HPV diagnosis is that the diagnosis (or lack of a diagnosis) depends on the
opinions of the doctor that analyzes the cells. When a person is diagnosed with something that he/she
does not have, this is known as a false positive. When a person is not diagnosed with something
he/she does have, this is known as a false negative.
Different doctors may look at the same sample of cells and disagree as to whether HPV is present. This
can lead to false negatives and false positives. Another problem is that up to 80% of the collected cells
remain in the collection device and are not analyzed. This can lead to false negatives because the
doctor may not be analyzing the sample of cells where the HPV is located. Fifty to seventy percent of
false negatives are due to the collected sample not being good enough. The sample that is collected
may have poor quality due to interference from blood, inflammation, or mucus (a thick, slippery fluid).
DOES THE PRESENCE OF GENITAL WARTS INCREASE THE CHANCES OF DEVELOPING
CERVICAL CANCER?
The presence of warts on the outside of the genitals does not increase the risk of cancer of the cervix.
Women with warts on the outside of the genitals do no need to go for a colposcopy or other special
tests if the Pap smear does not show any abnormalities. Please see the earlier section for a description
of a colposcopy and Pap smear.
WHAT DOES HPV LOOK LIKE?
When HPV is examined under a microscope it has 20 triangular surfaces with equal sides. It is circular
in shape and is about 55 nanometers in width. A nanometer is a very tiny unit of length equal to one
billionth of a meter. A meter is approximately 39 inches. A picture of HPV is shown to the right:
HOW IS HPV TREATED?
There is currently no specific way to cure or decrease an HPV infection. However, about 20-30%
cases of HPV go away without treatment. This is because the body's natural defense system can
sometimes fight off HPV within three to six months. Subclinical forms of HPV that only show up on a
Pap smear are likely to go away.
As was mentioned earlier, high-risk types of HPV can lead to flat abnormal growths of tissue that are
different from the characteristic appearance of warts. Treatment involves eliminating these abnormal
tissues. If these tissues are not removed in patients, a small percentage will go on to develop cervical
cancer. Genital warts usually disappear without treatment within 2 years, however, some new warts
may appear. Nongenital skin warts usually go away within 2 years. This section is divided into surgical
approaches to treatment and medication approaches.
SURGICAL APPROACHES:
Warts and abnormalities in tissues caused by HPV can be destroyed by cutting them out, applying
below-freezing temperatures to them (known as cryosurgery), applying heat and/or electrical currents,
or by using lasers or intense lights (see below for more details). More specific details about these
methods are provided below. When warts are frozen off (cryosurgery), it is done with a chemical
known as liquid nitrogen. A cotton tipped applicator (known as a cryoprobe) is used to place this
substance onto the patient. Liquid nitrogen can also be sprayed onto the patient. Besides liquid
nitrogen, gases such as nitrous oxide and carbon dioxide can be used to cause a freezing effect.
Cryosurgery is a quick and effective way to treat simple HPV disease. It is good at treating simple skin
warts and cervical dysplasia, which is a pre-cancerous condition that can develop into cervical cancer.
The water inside of the cells that make up the warts are frozen, which is what leads to their
destruction. The procedure can be painful and feel like a burning sensation. Medication to numb the
area where the warts are present is usually not needed.
There are two main ways that cryosurgery is performed: the single freeze method or the freeze-thaw
method. The single freeze method is just what it sounds like - the abnormality is frozen once. The
freeze thaw method, which is more painful yet more effective, involves freezing the abnormality until 5
millimeters of surrounding skin or mucous membranes is frozen. The skin will turn white from the
freezing and the skin is allowed to thaw. A second freezing is applied if the patient can tolerate it.
Within 24 hours, a thin-walled blister forms over the frozen area. After 2 to 4 cryosurgery treatments
over a period of 6 to 12 weeks, about 75 to 80% of patients no longer have warts. However,
cryosurgery may need to be performed multiple times to remove warts in some patients.
Cryosurgery is not recommended by doctors for use in the vagina. This is because the depth of tissue
destruction cannot be controlled in the vagina and can thus result in damage to nearby structures, such
as the urinary bladder. The urinary bladder is a hollow, muscular organ in the body that collects and
temporarily holds urine (pee) until it is ready to leave the body. Cryosurgery is considered safe with
pregnant women because the substance used to freeze the tissue is not systematically absorbed by
the body.
The use of electrical currents to destroy abnormal tissue (known as electrosurgery) can work by
sealing off blood vessels. There are different types of electrosurgery. One type uses a needle to
deliver the electric current. This form of electrosurgery is most effective with warts on the outside of
the genitals.
Another type of electrosurgery is known as Loop Electrosurgical Excision Procedure (LEEP). LEEP
uses a thin wire loop attached to an electric generator to deliver painless electric current that is used
to cut away and vaporize affected tissue. LEEP is usually used to treat squamous intraepithelial
lesions (see above) of the cervix. It is also used to remove large warts on the outside of the genitals.
Electrosurgery usually requires medication to numb the local affected area. If the equipment is
available, the procedure can be performed on an outpatient basis. Electrosurgery and laser surgery
produces smoke. Research has found traces of HPV DNA in the smoke plumes after electrosurgery.
Thus, procedures need to be used to prevent inhaling the smoke.
Laser surgery is often used for warts that have not responded to other forms of treatment. It is usually
not used as the first approach to remove abnormal tissues related to HPV. The advantage of laser
surgery is that the laser can be controlled very well and as a result, destruction of healthy tissue that is
next to the abnormal tissue can be largely avoided. Laser surgery is good at treating warts of the
vagina, warts around the urethra, and squamous intraepithelial lesions of the vagina. The urethra is a
tube shaped structure in the body that drains urine from the bladder.
Mohs surgery can also be performed as a treatment. Mohs surgery is a highly specialized form of
surgery for the total removal of skin cancers. Mohs surgery is most likely to be used in cases where
the doctor needs to be very careful about how much tissue is actually removed. Mohs surgery can be
particularly helpful in managing verrucous carcinomas. Verrucous carcinomas are carcinomas (see
above) of the squamous cells that have a bumpy, wart-like appearance. Verrucous carcinomas are
common in the mouth and penis.
The procedures discussed above can be used to destroy other types of abnormal tissue caused by
HPV. Surgery to remove warts can cause scarring. Also, treatment of genital warts does not affect the
development of cervical cancer. Surgery is usually only used when a large number of warts are present
or when a large area of the body is affected with warts that continue to return. The reason for this is
that surgery is time consuming, requires the use of more equipment (compared to applying medicated
gels on the warts), and sometimes requires the use of local anesthesia. Local anesthesia refers to
when a specific part of the body is numbed with medication.
Another procedure that uses heat to destroy affected tissue is the Cavitron Ultrasonic Surgical
Aspirator (CUSA). The CUSA device produces special types of sound waves that produce heat and
small vapor-containing bubbles or spaces in tissues. CUSA is especially useful in treating extensive
warts of the anus and genitals.
No one method to remove or treat warts or abnormal growths is considered to be superior to another
and multiple techniques over the course of weeks to months may be needed to get rid of them. No
single method cures warts and as such, they may reoccur. Each technique has advantages and
disadvantages, which should be discussed with the doctor.
The method chosen to remove warts or abnormal growths depends on several factors such as the
number, size, location, and structure of the abnormalities. The cost of the procedure, patient's
preference, experience of the health care provider, and adverse effects of the procedure are also
important factors to take into consideration. If significant improvements have not occurred after three
treatments or if the warts are not completely gone after 6 treatments, a different type of treatment is
used. The cutting off of warts is often used to remove large warts that have not improved with
treatment.
MEDICATION APPROACHES:
All medication that is used to treat HPV is applied to the affected tissue in a liquid or cream form. Pain
in the area where the medication is applied is a common side effect of these types of medications. The
medications are not meant to be applied to mucous membranes. The doctor should be aware of which
types of abnormalities related to HPV can be treated with the medications, and which cannot.
There are two main type of medications that are used to treat HPV. The first type is known as an
immune response modifier. These drugs work by improving the functioning of the body's immune
(defense system). These medications are mainly used to treat warts on the outside of the anus and
genitals. Examples of these drugs are interferon alfa and Aldara.
The second type of medications used to treat HPV are called cytotoxic agents, meaning that they are
drugs that kill cells. Examples are podofilox, podophyllin, 5-fluorouracil (5-FU), salicylic acid,
trichloroacetic acid (TCA), bichloroacetic acid (BCA), and salicylic acid. The last three drugs are useful
in the treatment of warts that are present on the skin, but not the genitals. All of these medications are
described in more detail below.
Interferon (also known as alpha interferon) is mostly used to treat warts that have returned after
treatment by traditional methods (such as freezing them or burning them off). Interferon is a type of
drug that decreases the reproduction of certain viruses and increases the number of natural killer cells
in the body. Natural killer cells are types of lymphocytes that help form the body's defense system. A
lymphocyte is a type of white blood cell present in the blood. White blood cells help protect the body
against diseases and fight infections.
A doctor injects interferon with a needle directly into the bottom center of warts. For large warts, this
medication may be injected in several parts of the wart. This is done three times a week for several
weeks. Research by the National Institute of Allergy and Infectious Diseases has shown that half of
the patients had their warts go away when injected with interferon.
Interferon usually works best by weeks 4 through 8, after the first course of treatment. For some
patients in which the warts have not gone away by 12 to 16 weeks, a second course of treatment with
interferon may be needed. Additional treatments of interferon with the same dosage may be need if the
patient has 6 to 10 warts. Up to 5 additional warts can be treated with each course of interferon.
Additional treatments with interferon may be needed if the patient has more than 10 warts.
Aldara (imiquimod) is used to treat warts of the genitals and anus. Aldara works by increasing
chemicals in the body known as cytokines, which produce various substances in the body that fight
viruses and destroy cancer cells. Aldara comes in the form of a cream. It is applied to the affected skin
area three times a week (approximately every other day). Aldara can be applied to the body by the
patient. It is removed through washing with mild soap and water, 6 to 10 hours after it is applied.
Doctors recommend that treatment with Aldara not last for longer than 16 weeks. Aldara is often useful
in patients who have not responded to other forms of therapy.
Medications containing about 20% of podophyllin (a resin that comes from type of plant called the
Mayapple) can be used to treat genital warts. Podophyllin contains a substance known as
podophyllotoxin that stops cells from growing at an early stage. Podophyllin is applied to affected
tissue areas by doctors, who are careful to avoid letting it contact healthy tissue. The first time the
medication is applied involves having it stay on the body surface for 30 to 40 minutes. Future
applications can be from 1 to 4 hours.
Podophyllin needs to dry thoroughly after it is put on. This medication is usually removed with alcohol
or soap and water about 7 hours after it is put on. The medication is applied on a weekly basis until the
warts disappear. It can be used for as long as six weeks. Doctors recommend against using
podophyllin to treat large warts or many warts at once. Doctors do not use podophyllin to treat warts
affecting mucous membranes, such as mucous membranes of the cervix and walls of the vagina.
Podophyllin can be manufactured or purified into a lotion or gel format. The lotion is also known as
podofilox lotion. The gel is known as podofilox gel and can be applied by the patient. Application of the
gel or lotion visibly destroys the wart tissue. Podofilox is normally used to treat warts on the outside of
the genitals.
Podophyllin is normally applied to the affected body part twice a day for three straight days. The drug is
then discontinued for four straight days and the cycle is repeated again (up to 4 cycles) until there are
no visible warts. This drug is used for a maximum of four, three-day cycles. Podophyllin can be applied
to the body by the patient. However, the person prescribing the drug should show the patient how to
use it properly and advise the patient how much is too much to put on at once.
Warts can be treated with creams that contain 5% of 5-fluorouracil (abbreviated 5-FU and sometimes
known as Efudex). The cream is commonly referred to as flourouracil cream. 5-FU is one of the most
common drugs used to treat cancer. It works by preventing cells from making and repairing DNA (see
above) and RNA (a substance in a cell that is important in making proteins). This action creates a
deficiency of thymine (a part of DNA), which causes unbalanced cell growth and cell death.
Although 5-FU is not formally approved to be used against warts, it has been shown to be helpful in
treating some genital warts. The cream is applied sparingly, 1 to 3 times a week, and may be used up
to 10 and 12 weeks. 5-FU should be prevented from contacting healthy tissue. 5-FU should be allowed
to dry thoroughly. The dried cream is removed 3 to 10 hours after it is applied.
Trichloroacetic acid (TCA) is also used to treat warts. TCA is a colorless drug that shrinks tissues and
helps decrease the growth of tiny organisms. Another powerful chemical, known as bichloracetic acid
(BCA), can be applied to all types of skin warts to destroy them. TCA and BCA help loosen and shed
the outer layer of the skin, where warts are present. TCA and BCA rapidly penetrate the skin and burns
skin, keratin, and other tissues, much like cryotherapy and electrosurgery does (see above). Keratin is
a type of tissue that is a main part of the top layer of skin.
A liquid that contains about 80 to 90% TCA (or BCA) is placed onto warts by a doctor on a weekly
basis until they disappear. As the acid dries, a white frosting develops. TCA or BCA is usually removed
about 7 hours after it is put on. Doctors do not use TCA to treat warts affecting mucous membranes,
such as mucous membranes of the cervix and walls of the vagina. Salicyclic acid is another type of
medication that works similarly to TCA and BCA. It can be purchased without a prescription and is
applied by the patient to treat skin warts that are on the skin but not on the genitals.
HPV that does not cause warts, but is only detectable by the diagnostic tests mentioned above may be
impossible to get rid of. Thus, in some cases, the HPV virus can be carried for life. Because HPV is
always present, the warts may return in the future. For example, HPV that is present (but not causing
warts) in healthy tissue that is next to a removed wart can become activated in the future. The
activation of the virus in the healthy tissue can cause a new wart to form.
As always, it is important to check with the doctor to determine which drugs are safe to take during
pregnancy. Doctors do not recommend using 5-FU, podophyllin, and podofilox during pregnancy.
Podophyllin and podofilox can be absorbed through the skin and cause birth defects.
WHAT KIND OF DOCTORS MIGHT I SEE IF I HAVE HPV?
There are many types of doctors that one could see if a person has HPV. The type of doctor that one
sees will depend on the complications or problems associated with this virus. In most cases, a woman
who is getting checked for HPV would go to an OB/GYN (obstetrician and gynecologist), which is a
doctor that specializes in obstetrics and gynecology.
Obstetrics is the science that deals with the care of women and their fetuses (developing babies)
during pregnancy and childbirth, and during the events that come before and soon after birth.
Gynecology is the study of the health care of women, including diseases and normal physical care of
the female reproductive system.
A doctor that specializes in cancer of the female reproductive system will need to be consulted if
cancer is present. This type of doctor is known as a gynecologic oncologist. Gynecologic oncologists
are also helpful in managing squamous intraepithelial lesions (see above) in the genital area. They are
also good at managing warts of the cervix that grow outwards and in managing giant warts.
An otolaryngologist (ear, nose, and throat doctor) may see the patient to help manage papillomas in the
oropharynx (described earlier). A urologist (doctor that specializes in the urinary system of males and
females and the male reproductive organs) can help manage HPV that has affected the urinary system.
The urinary system is the part of the body that deals with the formation and excretion of urine. To
excrete means to release from the body as waste.
If surgery needs to be performed on the anal area to remove warts or cancer, a specialist who
operates on this part of the body (known as a colorectal surgeon) may be consulted to help with the
case. A doctor that specializes in infectious diseases may need to be consulted if the patient has HPV
and decreased body defenses.
A dermatologist (skin doctor) may be used to help treat epidermodysplasia verruciformis (EV). See the
earlier section for a description of EV. A skin doctor may also be used to help clarify the diagnosis of
HPV in cases in which there are bleeding warts, birthmarks, or unusual-looking hairy warts present.
The reason this is important is because these warts or birthmarks can be confused with HPV.
Dermatologists may also be used to help with the surgical removal of warts or cancer if he/she has
special expertise in a type of surgery that might be helpful to the patient. An example would be a
dermatologist that specializes in Mohs surgery (see above).
CAN HPV BE PREVENTED?
The only way to prevent contracting HPV is to avoid the virus altogether. This is difficult to do since
HPV is the most common sexually transmitted disease in the United States. The chances of
contracting HPV can be reduced by not having sex or by using spermicides (substances that kill
sperm). Sperm is the male sex cell that joins with the female egg to produce offspring.
Reducing or avoiding risky sexual activity (such as reducing the number of sex partners) can decrease
the chance of developing HPV. Having sex with condoms made of latex or polyurethane may decrease
the risk of developing conditions related to HPV, such as genital warts and cervical cancer. Latex and
polyurethane are two substances that help make flexible materials.
Condoms do not offer full protection from HPV because the virus may be found on parts of the body
that is not protected by the condom, such as the anus. However, they may reduce the risk of getting
HPV when used correctly and consistently. Condom use has also been associated with decreased risk
for diseases related to HPV, such as cervical cancer.
Doctors recommend that people avoid having contact with partners that have genital warts, until the
warts are treated. This can decrease the chance of getting HPV. It is important to mention that cervical
cancer, one of the possible results of HPV infection, can easily be prevented by going for regular
check-up visits to the doctor.
HOW MANY PEOPLE DIE FROM CERVICAL CANCER?
Approximately 4,900 women in the United States die from cervical cancer each year. There are about
15,700 cases of cervical cancer a year in the United States.
HOW IS HPV CLASSIFIED?
HPV is classified as a virus in the family known as Papovaviradae. It is in the genus Papillomavirus. In
science, a genus is a specific group that is part of a family. Thus, there are different types of
Papillomoavirus (HPV being one of them) in the family Papovaviradae.
As a comparison, there are many different types of baked goods, just like there are many different
types of viruses. One group of baked goods is cookies. In our comparison, cookies are like a family. In
the family of cookies are chocolate chip cookies. In this case, chocolate chip cookies are a group of
cookies that are part of the family of cookies. Thus, in our comparison, the chocolate chip cookies are
like a genus.
DO OTER ANIMALS BESIDES HUMANS GET HPV?
No other animals besides human beings are known to get HPV.
WHAT ELSE IS HPV KNOWN AS?
HPV is also known as infectious papilloma virus.
WHAT IS THE ORIGIN OF THE TERM, HUMAN PAPILLOMAVIRUS?
Human papillomavirus comes from the Latin word "humanus" meaning "a man," the Latin word "papula"
meaning "a nipple," the Greek word "oma" meaning "tumor," and the Latin word "virus" meaning
"poison." Put the words together, and you have "a man a nipple tumor poison."