MedFriendly®
Spondylosis is a degenerative disorder that may cause loss of spinal structure or
functioning. Typically, there is stiffening or fixation of a vertebral joint as the result
means referring to vertebrae, which are bones that form an opening in which the
spinal cord passes. A joint is a place where two bones contact each other. The
vertebral bones are stacked one on top of another as shown in the second
picture below. Each individual bone that makes up the vertebrae is called a
vertebra. The main part of this bone is called the vertebral body. In between the
vertebrae are flat, cushiony disks (known as intervertebral disks) that act as
shock absorbers. These disks are represented by the red areas.
ARE THERE DIFFERENT TYPES OF SPONDYLOSIS?
The location and severity of spondylosis varies from person to person. There are three main types of
spondylosis, with the first two being the most common. If you’re seeking expert care, consulting Long
Island spine specialists can help diagnose and treat your condition effectively.
CERVICAL SPONDYLOSIS: This is any process in which the cervical spine (the part of the spine by
the neck) degenerates and produces narrowing of the spinal canal. The spinal canal is the space
between the spinal cord and the bony structure that surrounds it. Narrowing of the spinal canal can
compress the spinal cord and spinal nerves. The structure of the cervical spine is very complex. Since it
has a wide range of motion, the cervical spine is prone to disorders associated with degenerative
changes.
"Where Medical Information is Easy to Understand"™
LUMBAR SPONDYLOSIS: This is when there is any narrowing of the spinal canal in the lower back
(lumbar) region. Spondylosis affects the lumbar spine in people over age 40. Pain and morning stiffness
are common complaints when this spinal region has been affected. Usually, more than one vertebra is
involved. Because the lumbar spine carries most of a person's weight, pain may accompany physical
activity when degenerative forces weaken the structure of this area. This is especially likely during
repetitive movements such as lifting. Sitting for prolonged periods of time can cause pain and other
symptoms due to pressure on the lumbar vertebrae.
THORACIC SPONDYLOSIS: This is when there is any narrowing of the spinal canal behind the thoracic
region (the area behind the upper to middle part of the chest). The pain associated with this condition is
typically caused by flexing or hyperextending the back.
WHAT ARE SIGNS AND SYMPTOMS OF SPONDYLOSIS?
symptoms occur, pain and stiffness in the neck and lower back are common. Neck pain and neck
stiffness are especially likely in the morning or after performing recreational activities. Headaches can
occur, especially in the back of the head. Other symptoms include pain, weakness, and/or loss of
sensation in the arms, fingers, shoulders, and legs. Some people experience a sensation of pain
spreading down from the arms. Additional symptoms include movement difficulty, imbalance, buzzing in
the ears, loss of bladder control due to pressure on the spinal cord, inability to retain feces (poop),
difficulty swallowing, and muscle spasms (involuntary movements) around the spine. In the most severe
cases, severe impairment and paralysis (loss of movement and/or sensation) can occur.
WHAT CAUSES SPONDYLOSIS?
Spondylosis is mainly caused by aging. As people age, certain biological and chemical changes cause
tissues throughout the body to degenerate. In the spine, the vertebrae (spinal bones) and intervertebral
disks degenerate with aging. As was mentioned earlier, the intervertebral disks are cushion like
structures that act as shock absorbers between the vertebral bones.
One of the structures that form the disks is known as the annulus fibrosus. The annulus fibrosus is made
up of the 60 or more tough circular bands of collagen fiber (called lamellae). Collage is a type of inelastic
fiber. Collagen fibers, along with water and proteoglycans (types of large molecules made of a protein
and at least one carbohydrate chain) help to form the soft, gel-like center part of each disk. This soft,
center part is known as the nucleus pulposus and is surrounded by the annulus fibrosus.
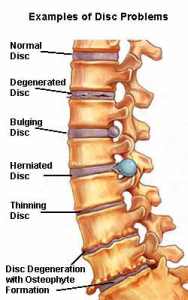
The degenerative effects of aging can cause the fibers of the disks to weaken, causing wear and tear.
Constant wear and tear and injury to the joints of the vertebrae causes inflammation in the joints.
Degeneration of the disks leads to the formation of mineral deposits within the disks. The water content
of the center of the disk decreases with age and as a result the disks become hard, stiff, and decreased
in size. This, in turn, results in strain on all the surrounding joints and tissues, causing the sensation of
stiffness. With less water in the center of the disks, they have decreased shock absorbing qualities. An
increased risk of disk herniation also results, which is when the disk abnormally protrudes from its normal
position.
Each vertebral body contains four joints that act as hinges. These hinges are known as facet joints or
zygapophyseal joints. The job of the facet joins is to allow the spinal column to flex, extend, and rotate.
The bones of the facet joints are covered with cartilage (a type of flexible tissue) known as end plates.
The job of the end plates is to attach the disks to the vertebrae and to supply nutrients to the disk. When
the facet joints degenerate, the size of the end plates can decrease and stiffen. Movement can stimulate
pain fibers in the facet joints and annulus fibrosus (see above). Furthermore, the vertebral bone
underneath the end plates can become thick and hard.
Degenerative disease can cause ligaments to lose their strength. A ligament is a tough band of tissue
that attaches to joint bones. In the spine, ligaments connect spinal structures such as vertebrae and
prevent them from moving too much. In spondylosis, one of the main ligaments (known as the
ligamentum flavum) can thicken or buckle, making it weaken.
Knobby, abnormal bone growths (known as bone spurs or osteophytes) can form in the vertebrae. These
changes can also cause osteoarthritis. Osteoarthritis is a disease of the joints that is made worse by
stress. In more severe cases, these bones spurs can compress nerves coming out of the spinal cord
and/or decreased blood supply to the vertebrae. Areas of the body supplied by these nerves may
become painful or develop loss of sensation and function. This explains why some people have neck
pain or arm pain. For example, when a bone spur compresses a nerve in the neck, arm weakness can
result. Poor coordination results because it is difficult to control muscles with poor sensations. Rarely,
bone spurs in the front of the cervical spine can cause difficulty swallowing. Since the neck is the
gateway to many nerves that lead to various parts of the body, when the neck is affected by spondylosis,
impaired functioning in those different body parts can result.
ARE THERE RISK FACTORS FOR SPONDYLOSIS?
Yes. The main risk factor for spondylosis is age.
HOW IS SPONDYLOSIS DIAGNOSED?
The first step towards diagnosis of spondylosis is a thorough review of the patient's personal and family
medical history and a detailed physical evaluation. A physical evaluation can tell a lot about the health
and general fitness of the patient. A physical exam can be done through a neurological examination. A
neurological examination formally assesses the patient's sensory symptoms such as pain, numbness,
and abnormal sensations (such as tingling). It can also assess motor (movement) functioning, especially
in the arms and legs. The degree that the patient can flex, extend, bend to the side, and rotate different
body pats are used to assess motor functioning. Examination by touch helps determine spinal
abnormalities such as tenderness and muscle spasms. Reasons for bowel and bladder changes can
also be examined through the physical exam. If the neurological examination shows abnormalities,
additional tests may be needed to understand the nature and extent of disease.
One of the most common tests used to diagnosis spondyolsis is an x-ray to examine the condition of the
neck bones. An x-ray can tell if there has been a decrease in disk size and if bone spurs are present.
Sometimes, a discography is used in which colored dye is actually injected into the disk so that the disk
shows up more clearly on the x-ray. A discography is useful because it can help identify the exact source
of pain. A similar test is called the facet joint block test, in which medicine is injected to numb a joint. If
the injection helps to reduce pain, the doctor assumes he/she has found where the pain is coming from.
Yet another common test is known as a myelogram, which highlights the condition of the spinal cord and
nerves by injecting a special dye into the spine.
More advanced and sensitive techniques are used in more serious cases. Two of these tests are known
as CT (computerized tomography) scanning and MRI (Magnetic Resonance Imaging). CT scanning is an
advanced imaging technique that uses x-rays and computer technology to produce more clear and
detailed pictures than a traditional x-ray. MRI scans produce extremely detailed pictures of the inside of
the body by using very powerful magnets and computer technology. MRI is better than CT scans at
evaluating soft tissue, ligament, disk, and nerve abnormalities. CT scans are better than MRI at
evaluating bones (such as the bony changes associated with spondylosis). Lastly, electromyography
(EMG) is sometimes used to help diagnose spondylosis because it measures electrical impulses to
assess the health and strength of muscles and the nerves that control muscles.
Once the tests are completed, the doctor compares the patient's symptoms to the findings to formulate a
diagnosis and treatment plan. Also, the test results will provide a baseline from which the doctor can
monitor the patient's progress.
HOW IS SPONDYLOSIS TREATED?
To begin with, the doctor may suggest rest because in mild cases the symptoms sometimes go away
without medical treatment. However, a balance between rest and mild to moderate physical activity is
often recommended, except in some severe cases. Regular, gentle exercise can help ease neck pain
and stiffness. Physical therapists are often consulted to develop the best exercise routine. Physical
therapy is sometimes attempted to strengthen and rehabilitate the muscles and joints by the spine and
belly. Strengthening muscles near the belly helps provide support to the spine. Physical therapists can
also use electrical stimulation and heat to reduce symptoms such and pain and muscle spasms.
Sometimes, isometric exercises are used when movement is painful or difficult. Isometric exercise
involves tensing a muscle and holding it in a stationary position while maintaining the tension. Isometric
exercises are especially helpful to people recovering from injuries that limit movements. In general,
exercise helps increase strength, flexibility, and range of movement.
Swimming or hydrotherapy can help overcome stiffness. Hydrotherapy is the use of water to treat
disease. If such an approach is taken, it is more likely for the discomfort to improve with time, but the
stiffness may remain. Lifestyle changes may also be needed such as quitting smoking, losing weight,
and changing jobs (such as avoiding manual labor). Strong medical reassurance by the doctor and
recommendations on how to improve posture and physical fitness can also be helpful.
In serious cases, the doctor may ask the patient to wear a neck collar or neck brace so that the neck
becomes stabilized and rested to reduce pain. To stabilize and prevent stress on the lower back, a
lumbar (lower back) support belt may be suggested. During the sudden onset of symptoms, medications
may be prescribed for a short period of time to relieve pain, help muscles relax, and reduce
inflammation.
In the most serious cases, traction and/or surgery may be necessary. Traction is a treatment that uses a
pulling force to keep a joint in place, prevent or decrease muscle spasms, or to hold the end of broken
bones in place. In spondylosis, traction helps to reduce pressure by attaching a device to the patient's
head and pulling up on it by using a system of pulleys and weights. The traction device is usually applied
a few times a day and can be used while sitting or lying in bed. In some severe cases, bed rest for one or
two weeks might be necessary.
It should be mentioned that surgery is seldomly used to treat spondylosis and that it is only used as a
last option. Whether surgery can be used in severe cases depends on the patient's age, lifestyle,
occupation, how long the condition has been present, the degree and nature of the damage, and if motor
or sensory symptoms are present. Surgery involves removing the abnormal bony growths and/or
stabilizing the neck by fusing the vertebrae together (known as spinal fusion). A spinal doctor is needed
to determine if surgery is necessary.
WHAT IS THE PROGNOSIS FOR PEOPLE WITH SPONDYLOSIS?
The answer to this depends on the severity of the case. As was mentioned in the last section, mild cases
may go away without treatment. In fact, about 75% of cases go away without having to resort to surgery.
If medication is required, chances of recovery improve by taking medications as directed and reporting
side effects to physicians. Prognosis generally improves by following the prescribed physical therapy
program, stopping smoking, keeping an average weight, and avoiding heavy lifting or other situations
that increase pain or other symptoms.
In severe cases, long-lasting and permanent disability may result. Neck pain, for example, can be long-
standing and there can be worsening loss of muscle function and sensation over time. Long-lasting
disability is rare, however. The doctor and/or physical therapist will be able to provide strategies to
reduce the risk of further back problems and whether or not any restrictions in work and/or recreational
activities should be present.
WHAT ELSE IS SPONDYLOSIS KNOWN AS?
Spondylosis is also known as spinal osteoarthritis.
WHAT IS THE ORIGIN OF THE TERM, SPONDYLOSIS?
Spondylosis comes from the Greek word "spondylos" meaning "vertebra" and the Greek word "osis"
meaning "condition." Put the words together and you have "vertebra condition."
Spondylosis